The post What does the Congressional Budget Office research show about premium support? first appeared on SEONewsWire.net.]]>In 2013 the Congressional Budget Office (CBO) researched how premium support, as suggested by House Speaker Paul Ryan’s “A Better Way,” would impact the federal budget, beneficiaries’ payments and choices. The results of their research revealed that under the two different proposed premium support plans, that both would “reduce federal spending for Medicare net of beneficiaries’ premiums and…
The post What do the changes to Medicare mean? first appeared on SEONewsWire.net.]]>The new administration plans to push health care reform, and in the process overhaul Medicare, by eventually implementing what they refer to as premium support. What does that mean for Americans? It means that premium support would increase competition among health care providers, thus offering beneficiaries the choice of where to spend their money when choosing providers. House Speaker Paul Ryan…
There will be those who come to you after dealing with another agent or trying to keep up with all the Medicare changes on their own. Their story might go like this: they thought they had all the bases covered and signed up in time, only to discover they forgot to enroll in Part D. Now what?
Part of your job as an insurance expert is to offer various kinds of help to those needing your assistance. While you cannot enroll seniors in Part D, if they missed the deadline, you may offer them some other alternatives. One of which would be to inform them about pharmacy programs.
Many states have very large superstores with pharmacies that offer pharmacy discount programs. If a senior signs up for such a program, they are usually able to buy some of the prescription drugs they need for a discount. Although there are minimal initial fees the discounts received offsets those fees. Giving good customer service is also a good way to keep loyal clients.
The post Further options for seniors if they miss out on enrolling in Part D first appeared on SEONewsWire.net.]]>The Trump Policy Analysis Group (TPAG)1 has convened to consider probable changes in law that will affect older Americans and those with special needs. Initial TPAG focus is on entitlements, public benefits, tax, special needs planning, and veterans’ benefits.
We used a three-fold analysis:
- Stated policy (declared Trump policies and those of the Republican Congressional Leadership);
- “Realpolitik” (circumstances and factors rather than explicit ideology, often considered “pragmatism”); and
- Educated speculation (based largely on experience and knowledge of TPAG members who have been leaders in these fields for decades).
STATEMENT OF PURPOSE
On January 20, 2017 both the White House and both houses of Congress will be in Republican hands, not seen since 2006. As president Obama said shortly after being elected in 2008, elections have consequences. We acknowledge this reality.
During the long and divisive campaign, differences in priorities and agendas between the major parties, particularly in social and health policy, were greater than in any recent election. In our opinion, the uncertainty and challenges now facing seniors, disabled, and medically needy Americans are unequaled and unsettling.
Our goals are twofold. First, to objectively analyze real and probable changes in government policies that directly impact older Americans and Americans with disabilities. Second, to identify planning and other steps these populations should take to preserve or, ideally, to increase quality of health care and quality of life.
SOCIAL SECURITY AND MEDICARE
President-elect Trump has consistently stated that the Social Security and Medicare programs are to remain intact and (presumably) solvent. How solvency would be achieved in light of impending bankruptcy of both programs (Medicare long before Social Security) remains to be seen. Government and non-government economists only disagree about when insolvency will occur, not if it will occur. As one of their proposals to counter insolvency, Trump and Congressman Ryan (Speaker of the House) are promoting Social Security and Medicare privatization.
The Affordable Care Act took some steps designed to extend the solvency of Medicare. Trump, as President-elect, announced that he would keep parts of the Affordable Care Act but did not explain how he would pay for it. With so many members of younger generations convinced that Social Security will not be there for them, preservation of the fiscal health of both Social Security and Medicare is one of the main challenges facing this Administration.
MEDICAID
1. Rising Fears of Significant Restrictions
A significant majority of Americans are seriously worried about the cost of health care and long term care, in particular. Restrictions on benefits and legislative changes that restrict or limit access to government programs such as Medicaid can only heighten such fears.
2. The Trump and Ryan Block Grant Proposal
Currently, Medicaid is administered at the federal level by the Center for Medicare and Medicaid Services (CMS). While each state has its own state Medicaid Plan, there are mandates and there are constraints.
Block grants, which were first proposed by then Speaker of the House Newt Gingrich in 1995, presumably mean that each state would receive a certain number of Medicaid dollars. Each state would then decide how to utilize and spend those dollars. In some states, little would change. In other states, changes could be profound. For individuals who may rely on Medicaid, this is a time of uncertainty and concern. This means, in turn, that planning needs will vary from state to state.
TPAG is aware of some details and elements of proposed plans. Some are designed to restrict protective planning – to make it much more difficult for older Americans to protect their homes and other assets while qualifying for Medicaid, particularly in a long-term care setting. Planning challenges could therefore become dramatically more difficult. Increasingly, older Americans and their families will need up-to-date information and advice to understand and qualify for needed services. This will be particularly true for the majority of older Americans who will need home care services and who need to reside in skilled nursing facilities.
Americans with special needs and their families face as many worries, including concerns about possible reductions in protections and services.
TPAG believes that planning will increasingly involve multiple generations to enhance quality of life, quality of care, and asset protection.
3. Protection of Family Assets: Focus on Protecting the Family Residence
The vast majority of older homeowners will view protection of the residence as a core value, a legacy for future generations. Appropriate legislation must be preserved. Appropriate planning steps must be taken, particularly in light of possible changes in Medicaid, the only federal program that can subsidize or pay for the cost of skilled nursing care. No specific proposals to threaten existing tax and Medicaid protections for the residents have yet emerged.
TAX PROPOSALS – GIFT, ESTATE, INCOME, AND CAPITAL GAINS
1. Gift and Estate Tax
President-elect Trump calls for the elimination of gift and estate tax, perhaps replaced by a “mark to market” tax of capital gains at death. Perhaps a compromise package will not eliminate the tax but will significantly increase the level of estate and gift tax protection. Note that the current level of federal protection is historically high at $5,450,000 per person. If any estate tax remains, it would likely be reduced from the current 40% tax rate.
2. Capital Gains Tax
Different proposals have been proffered by President-Elect Trump, Speaker Ryan and others regarding limitations on “stepped up basis” upon an individual’s passing. For some families, this could result in net tax increases.
For high-end practitioners, those who focus on avoiding estate tax, the challenges are obvious. The number of individuals requiring such sophisticated planning will, at best, dramatically diminish. For most older Americans, the avoidance of estate taxes will have little or no impact from a tax planning perspective and the focus will shift to income taxation. Further, the impacts on entitlements and family financial security could be profound.
3. Corporate and Individual Income Tax
Corporate and individual tax rates for higher earners, in particular, would be substantially reduced. The long-term impact – beyond the obvious increase in after tax income, is impossible to predict. As with most modeling and forecasting, projected outcomes depend on presumptions.
AMERICANS WITH SPECIAL NEEDS
No proposals have yet been made that would directly affect services for special needs children and adults. Medicaid block grants could adversely affect special needs residents of states that decide – at the state level – to reallocate or otherwise restrict funding for both governmental and non-governmental providers. The reach of Medicaid block grants could significantly reduce or even eliminate the benefit of special needs trusts which maximize assets for the person with a disability.
Additionally, it is possible that support for expanded charter schools and school choice could expand options. This has become more probable than just possible what with Trump’s appointment of Betsy DeVos, as Secretary of Education, an outspoken advocate for charter schools and the dismantling of publicly funded schools. Many special education advocates fear these expanded options could come at a price of diminishing procedural and substantive protections of the Individual with Disabilities Education Act (IDEA), and even reduce or remove the funding formula that follows eligible individual students with special needs under IDEA).
VETERANS’ BENEFITS
President-elect Trump is presumably supportive of maintaining and perhaps expanding services for veterans. At the same time, proposals that predate the election have been introduced that could restrict access to needed programs, such as Aid and Attendance, which provides financial assistance for veterans and spouses of veterans who need higher levels of home care assistance. While new legislative and perhaps regulatory restrictions could make it more difficult for veterans and their spouses to obtain benefits, proactive planning will be an inevitable need across the nation.
LGBTQ PROTECTIONS
President-elect Trump has said that he accepts the United States Supreme Court decision effectively legalizing gay marriage. (His Vice President, Mike Pence, may have a different viewpoint.) The Supreme Court ruled that the U.S. Constitution guarantees the right for same-sex couples to marry in all 50 states creating uniformity across the nation in recognition of the rights of same-sex couples.
IN TIMES OF UNCERTAINTY, FAMILIES WILL PROTECT THEMSELVES
A core conclusion of TPAG is that families will become more insular, more protective of themselves, their assets, and future generations. They will be more focused on what they can control and truly value – their families – and less on public policies that are difficult to influence. This has myriad implications for attorneys, financial planners, and other professionals who work directly with America’s elders, those with special needs and their families. A premium will be placed on advance planning. Inevitably, this will increase involvement of younger generations. The demand for multi-generational planning – planning that involves and relies on involvement of children and grandchildren – will expand dramatically.
WHAT SHOULD YOU DO?
TPAG thoroughly understands that most Americans, and older Americans in particular, are fearful at this point in time. Above all, do not panic. The stock market panicked at the end of Election Day but soon resolved and moved higher than ever. TPAG believes that the stock market’s response to the election is a lesson for everyone: Learn, watch, be advised, and protect yourself and your family. The changes in store will take time.
TPAG’s goal and its purpose is to turn fear into hope. This is what good planning does.
TPAG will continue to be a source of balanced, objective information about developments at the national level. TPAG is working hard to track initiatives by President-elect Trump, Republicans and responsive proposals of Democrats.
TPAG will work hard to be “one step ahead.”
**Members of the TPAG group include Michael Gilfix of Palo Alto, California, Vincent J. Russo of Garden City, New York, Harry S. Margolis of Boston, Massachusetts, Frank Johns of Greensboro, North Carolina, and Tim Nay of Portland, Oregon.
 |
 |
 |
 |
 |
Co-Author: Letha Sgritta-McDowell
During the holidays, it is not uncommon for emergency rooms to see an increase in visits by the elderly population. As we know, the elderly are more susceptible to catching pneumonia due to their waning immune systems, falling due to lower body weakness and poor balance, combined with vision problems or home hazards like throw rugs and/or clutter that can be tripped over, and even medication mismanagement caused by having too many prescriptions to take or being prescribed a combination of medications by several different doctors that do not work together but against each other. With the rise of hospital admissions this time of year, come families who are thrust into a situation they have never experienced before; they are often worried, scared, and confused.
We often receive calls from family members trying to understand the processes for hospital admissions, rehabilitation services, and long-term care for their loved one. There are several points at which families can become easily confused. The first is upon discharge from the hospital. Hospitals are acute care facilities; meaning that a person’s stay is only temporary. For longer term rehabilitation and care while a person is recovering from an acute illness, this type of care is provided either at home or in an outside facility. Any number of terms are used at this juncture. Families may hear “rehab,” “skilled nursing,” “nursing home,” or simply “therapy.” The discharge planner at the hospital will offer you and your loved one options for this continuing care. For individuals who are recovering from an acute illness, this possible discharge to a nursing home is not permanent. This is merely a suggestion that the elderly person move to a facility where he or she can receive nursing services as well as all available therapy with the goal that they can recover enough to safely return home. For many seniors who live alone, a short rehabilitation stay is the safest way to receive the care they need. Understandably, many people would prefer to go home. The same therapy may be offered on an outpatient basis.
When evaluating outpatient rehabilitation instead of going to a nursing home, the individual and their family need to consider who will be able to take their loved one to any and all doctor’s appointments and therapy sessions as well as who will cook, clean, do laundry and assist the loved one with bathing, dressing and other essential daily activities. It requires a strong support system and/or the ability to hire private duty care providers to ensure a successful rehabilitation in the home. Therefore, when faced with this decision, it is important that the family consider all options. If a discharge to a facility is chosen but rehabilitation in the home later becomes feasible, that certainly can happen.
If an individual is discharged to a nursing facility but does not fully recover or if they have needs which will continue long after rehabilitation is finished, then they often face another stressful and confusing crossroads. If the individual was admitted to the hospital for three nights or more prior to their discharge to the nursing facility, then Medicare can pay for up to 100 days, so long as the patient responds to the therapy being prescribed by his or her doctor, or if the stay in the facility is necessary to maintain the individual’s current level of health and functionality. However, once the patient stops responding to therapy, refuses to participate, or if the care is not necessary to maintain his or her current level of health, representatives from the facility will discuss “discharge.” Unfortunately, the context of discharge at this stage is often not explained fully, and many family members assume that this discussion means their loved one is being sent home. As discussed earlier, for many the transition home is complicated and can be potentially dangerous for the senior. Understandably, the sense that an elderly person is being sent home when provisions are not available to assist them can cause family members to panic.
However, the discussion of discharge at this juncture simply means that the patient is no longer eligible for Medicare-covered rehabilitation services. If, after rehabilitation, the individual still needs assistance with bathing, dressing, walking, eating and other activities of daily living, then the family can (and should) request that their loved one transition to long-term care within the facility.
Many times we hear that family members were not provided options and were simply told that their loved one was being discharged. This often leads to family members scrambling to find care for their loved one. In other situations, when the family asks about staying longer, a facility representative may explain to the family that no beds are available or they cannot accommodate the care needs of the patient. There are laws in place which require the nursing facility to assist with a safe and appropriate discharge plan for the patient. If no beds are available at that facility and services and supports are not sufficient in the community, then the facility representative must find another facility which has an available bed and which can accommodate the person’s care needs. While looking for a suitable bed, the patient is allowed to stay at the same facility in their current bed.
The rules and regulations surrounding hospital discharge planning and discharge from Medicaid covered rehabilitation can be mysterious and, without proper understanding, can cause additional stress in an already emotional and stressful time. If you or your loved one find yourself in this position, you should immediately seek someone experienced with resident rights who can help navigate this process and develop a long-term care plan focused on developing a solution to the problem. The attorneys and staff of Hook Law Center are experienced and prepared to assist you or your loved one through this process. Please call us today to schedule an appointment to discuss your rights and options.
 Ask Kit Kat – Mickey, Our Own Star
Ask Kit Kat – Mickey, Our Own Star
Hook Law Center: Kit Kat, I hear that Hook Law Center has many employees who love pets. One in particular—Mickey—the beloved cat of Cynthia is making medical history. What can you tell us about her cat?
Kit Kat: Mickey is an 18-pound male cat who has just been diagnosed with gigantism or its scientific name of acromegaly. His length from head to tail is more than 3 feet! He is a beautiful brown tabby with white feet who is 10 years old. On January 11, 2017, he will turn 11. Anyway, he was gaining weight, and at one point he weighed in at 21 pounds, even though he was on a diet. Such a large figure caused him difficulty in jumping onto chairs, etc. When Cynthia took him to the vet, they treated him for arthritis and an underactive thyroid. Still the vet thought there might be something else affecting his condition. It was suggested that Cynthia collect a blood sample, and send it to a lab at Michigan State University in East Lansing, Michigan. Cynthia recently got the results. The suspected condition of gigantism was confirmed. This is an extremely rare condition in cats, caused by over production of the growth hormone (GH). It usually affects males around the median age of 11, so it looks unfortunately like Mickey falls into a classic case. He also displays some other common signs of the disease with his enlarged lower jaw and head.
Treatment can include radiation therapy. However, at this stage in his life and because of the severity of his case, the vet has not recommended anything other than to continue to address his arthritis and thyroid. Mickey is lucky he is in the home he is in. Cynthia and husband, Carl, have even built him a stand to hold his food and water bowls, so he doesn’t have to bend over so far. Eventually, he will undoubtedly succumb to heart disease or renal failure, though the latter is very common in cats as a whole, even those without gigantism. Cynthia and Carl will do their best to keep him comfortable and extend his life as long as possible. (http://www.cat-world.com/au/acromegaly-in-cats)
Distribution of This Newsletter
Hook Law Center encourages you to share this newsletter with anyone who is interested in issues pertaining to the elderly, the disabled and their advocates. The information in this newsletter may be copied and distributed, without charge and without permission, but with appropriate citation to Hook Law Center, P.C. If you are interested in a free subscription to the Hook Law Center News, then please telephone us at 757-399-7506, e-mail us at mail@hooklawcenter.com or fax us at 757-397-1267.The post ‘Tis the Season…for hospital admissions and long-term are planning! first appeared on SEONewsWire.net.]]>
Co-Author: Letha Sgritta-McDowell
During the holidays, it is not uncommon for emergency rooms to see an increase in visits by the elderly population. As we know, the elderly are more susceptible to catching pneumonia due to their waning immune systems, falling due to lower body weakness and poor balance, combined with vision problems or home hazards like throw rugs and/or clutter that can be tripped over, and even medication mismanagement caused by having too many prescriptions to take or being prescribed a combination of medications by several different doctors that do not work together but against each other. With the rise of hospital admissions this time of year, come families who are thrust into a situation they have never experienced before; they are often worried, scared, and confused.
We often receive calls from family members trying to understand the processes for hospital admissions, rehabilitation services, and long-term care for their loved one. There are several points at which families can become easily confused. The first is upon discharge from the hospital. Hospitals are acute care facilities; meaning that a person’s stay is only temporary. For longer term rehabilitation and care while a person is recovering from an acute illness, this type of care is provided either at home or in an outside facility. Any number of terms are used at this juncture. Families may hear “rehab,” “skilled nursing,” “nursing home,” or simply “therapy.” The discharge planner at the hospital will offer you and your loved one options for this continuing care. For individuals who are recovering from an acute illness, this possible discharge to a nursing home is not permanent. This is merely a suggestion that the elderly person move to a facility where he or she can receive nursing services as well as all available therapy with the goal that they can recover enough to safely return home. For many seniors who live alone, a short rehabilitation stay is the safest way to receive the care they need. Understandably, many people would prefer to go home. The same therapy may be offered on an outpatient basis.
When evaluating outpatient rehabilitation instead of going to a nursing home, the individual and their family need to consider who will be able to take their loved one to any and all doctor’s appointments and therapy sessions as well as who will cook, clean, do laundry and assist the loved one with bathing, dressing and other essential daily activities. It requires a strong support system and/or the ability to hire private duty care providers to ensure a successful rehabilitation in the home. Therefore, when faced with this decision, it is important that the family consider all options. If a discharge to a facility is chosen but rehabilitation in the home later becomes feasible, that certainly can happen.
If an individual is discharged to a nursing facility but does not fully recover or if they have needs which will continue long after rehabilitation is finished, then they often face another stressful and confusing crossroads. If the individual was admitted to the hospital for three nights or more prior to their discharge to the nursing facility, then Medicare can pay for up to 100 days, so long as the patient responds to the therapy being prescribed by his or her doctor, or if the stay in the facility is necessary to maintain the individual’s current level of health and functionality. However, once the patient stops responding to therapy, refuses to participate, or if the care is not necessary to maintain his or her current level of health, representatives from the facility will discuss “discharge.” Unfortunately, the context of discharge at this stage is often not explained fully, and many family members assume that this discussion means their loved one is being sent home. As discussed earlier, for many the transition home is complicated and can be potentially dangerous for the senior. Understandably, the sense that an elderly person is being sent home when provisions are not available to assist them can cause family members to panic.
However, the discussion of discharge at this juncture simply means that the patient is no longer eligible for Medicare-covered rehabilitation services. If, after rehabilitation, the individual still needs assistance with bathing, dressing, walking, eating and other activities of daily living, then the family can (and should) request that their loved one transition to long-term care within the facility.
Many times we hear that family members were not provided options and were simply told that their loved one was being discharged. This often leads to family members scrambling to find care for their loved one. In other situations, when the family asks about staying longer, a facility representative may explain to the family that no beds are available or they cannot accommodate the care needs of the patient. There are laws in place which require the nursing facility to assist with a safe and appropriate discharge plan for the patient. If no beds are available at that facility and services and supports are not sufficient in the community, then the facility representative must find another facility which has an available bed and which can accommodate the person’s care needs. While looking for a suitable bed, the patient is allowed to stay at the same facility in their current bed.
The rules and regulations surrounding hospital discharge planning and discharge from Medicaid covered rehabilitation can be mysterious and, without proper understanding, can cause additional stress in an already emotional and stressful time. If you or your loved one find yourself in this position, you should immediately seek someone experienced with resident rights who can help navigate this process and develop a long-term care plan focused on developing a solution to the problem. The attorneys and staff of Hook Law Center are experienced and prepared to assist you or your loved one through this process. Please call us today to schedule an appointment to discuss your rights and options.
 Ask Kit Kat – Mickey, Our Own Star
Ask Kit Kat – Mickey, Our Own Star
Hook Law Center: Kit Kat, I hear that Hook Law Center has many employees who love pets. One in particular—Mickey—the beloved cat of Cynthia is making medical history. What can you tell us about her cat?
Kit Kat: Mickey is an 18-pound male cat who has just been diagnosed with gigantism or its scientific name of acromegaly. His length from head to tail is more than 3 feet! He is a beautiful brown tabby with white feet who is 10 years old. On January 11, 2017, he will turn 11. Anyway, he was gaining weight, and at one point he weighed in at 21 pounds, even though he was on a diet. Such a large figure caused him difficulty in jumping onto chairs, etc. When Cynthia took him to the vet, they treated him for arthritis and an underactive thyroid. Still the vet thought there might be something else affecting his condition. It was suggested that Cynthia collect a blood sample, and send it to a lab at Michigan State University in East Lansing, Michigan. Cynthia recently got the results. The suspected condition of gigantism was confirmed. This is an extremely rare condition in cats, caused by over production of the growth hormone (GH). It usually affects males around the median age of 11, so it looks unfortunately like Mickey falls into a classic case. He also displays some other common signs of the disease with his enlarged lower jaw and head.
Treatment can include radiation therapy. However, at this stage in his life and because of the severity of his case, the vet has not recommended anything other than to continue to address his arthritis and thyroid. Mickey is lucky he is in the home he is in. Cynthia and husband, Carl, have even built him a stand to hold his food and water bowls, so he doesn’t have to bend over so far. Eventually, he will undoubtedly succumb to heart disease or renal failure, though the latter is very common in cats as a whole, even those without gigantism. Cynthia and Carl will do their best to keep him comfortable and extend his life as long as possible. (http://www.cat-world.com/au/acromegaly-in-cats)
Distribution of This Newsletter
Hook Law Center encourages you to share this newsletter with anyone who is interested in issues pertaining to the elderly, the disabled and their advocates. The information in this newsletter may be copied and distributed, without charge and without permission, but with appropriate citation to Hook Law Center, P.C. If you are interested in a free subscription to the Hook Law Center News, then please telephone us at 757-399-7506, e-mail us at mail@hooklawcenter.com or fax us at 757-397-1267.The post ‘Tis the Season…for hospital admissions and long-term care planning! first appeared on SEONewsWire.net.]]>

The post Nursing Home Residents Will Soon Have Greater Rights first appeared on SEONewsWire.net.]]>A rule change by a federal agency will provide nursing home residents with major new legal protections by preventing facilities from forcing disputes into arbitration.
The Centers for Medicare and Medicaid Services (CMS), part of the Health and Human Services Department, issued a rule preventing nursing homes from requiring that residents resolve disputes in arbitration rather than through a…

However, there is one big exception to the collateral source rule in Florida, and that is with regard to payments made by governmental agencies, such as Medicare or Medicaid. The general thinking is that while health or private insurance benefits are earned by a plaintiff with money from their own pockets – and shouldn’t be penalized for taking such initiative – those who obtain federal benefits as a matter of entitlement without actually earning it may not be entitled to the same protection.
In the recent case of Patchett v. Lee, the Indiana Supreme Court reached a similar conclusion. According to court records, the appeals court in this matter previously ruled that government reimbursement rates aren’t accurate reflections of the actual value of a health care service. However, the state supreme court reversed.
Plaintiff was injured in a crash for which the other driver admitted her negligent driving was the cause. However, the two parties disagreed on damages or, specifically, what was the reasonable value of plaintiff’s medical care.
Both parties agreed that Indiana laws permitted plaintiff to enter into evidence accident-related bills that totaled $88,000, and that was evidence those amounts were reasonable. However, they could not come to an agreement regarding whether defendant could introduce the reduced amount that was actually paid by the government-sponsored health care program – which amounted to a total of $12,000, which fully satisfied the outstanding balance at an 86 percent discount.
Plaintiff moved to prevent jurors from hearing this evidence, arguing that payments made by government insurers weren’t permitted under the state’s collateral sources rule. The court agreed, and also concluded that evidence of this would only serve to confuse the jurors. Although the court granted plaintiff’s motion, it certified an interlocutory appeal for review to the appellate court. The trial court stated that resolution of this issue was critical to the importance in this case – and others – concerning a jury’s determination of damages.
The appellate court affirmed the trial court’s grant of plaintiff’s motion, saying the reimbursed amount was indicative only of market negotiation, but wasn’t probative or reflective of the actual value of services.
Defendant appealed to the state supreme court, which reversed.
The court noted firstly that what is a “reasonable” amount for a health care service for personal injuries can be proved in a number of ways. One of those ways is to present medical bills that reflect charges for certain services. However, if one of the parties contests the reasonable amount of those charges, then there is going to be more to the story.
Common injury law precedent in Indiana held that the collateral source statute wouldn’t prohibit evidence of discounted amounts to determine what is a reasonable amount, so long as insurance isn’t mentioned. Where the trial court went wrong in this case was to assume this only meant that those amounts negotiated between a health insurance company and medical provider applied. For the first time, the court held, amounts paid by government-backed insurance may also be presented to the jury.
If you have been a victim of a traffic accident, call Chalik & Chalik at (954) 476-1000 or 1 (800) 873-9040.
Additional Resources:
Patchett v. Lee, Oct. 21, 2016, Indiana Supreme Court
More Blog Entries:
Schaefer v. Universal Scaffolding – Spoliation of Evidence in Construction Accident Lawsuit, Oct. 24, 2016, Car Accident Miami Lawyer
The post Patchett v. Lee – Collateral Source Rule Weighed first appeared on SEONewsWire.net.]]>The premiums, which represent the amount the policyholder pays the insurance company to maintain the effectiveness of the policy, can be deducted by the taxpayer, the taxpayer’s spouse and other dependents. The rules for tax-deductibility are somewhat different for a person who is self-employed. You can deduct the premium, provided you realized a net profit. It is not required that your medical expenses are greater than a specific percentage of your income.
However, there is a maximum premium amount that is deductible. This figure is dependent on the age of the plaintiff at the end of the year. Below are the caps on deductibility for 2016. Any premium amounts that exceed these restrictions are not deemed to be a deductible medical expense.
Age prior to the end of the taxable year / Maximum deduction for the year
- 40 or under / $390
- Over 40 but not over 50 / $730
- Over 50 but not over 60 / $1,460
- Over 60 but not over 70 / $3,900
- Over 70 / $4,870
The elder law attorneys at Hook Law Center assist Virginia families with will preparation, trust & estate administration, guardianships and conservatorships, long-term care planning, special needs planning, veterans benefits, and more. To learn more, visit http://www.hooklawcenter.com/ or call 757-399-7506.
The post Premiums for long-term care insurance can be a tax deduction first appeared on SEONewsWire.net.]]>True, insurance contracts are complex. However, that is not the real issue. Selling insurance is not so much about the actual contract as about the concept behind it – protection for an individual or family. A policy that takes care of loved ones “if” something happens, a Medicare supplement that is perfect for a customer and provides the care they need to stay healthy and happy, or an older grandfather who wants to make sure his family is not burdened with funeral and burial costs.
Selling protection to those that need it and those that do not yet know they need it or do not understand why insurance is necessary is the glue that holds your agency together. Education is a major component of what you do for a living (selling insurance) and why you want to help others understand that insurance is vitally important.
While you may prefer doing that in person, online marketing is a crucial component of any smart insurance agency marketing plan these days. It also opens the door to thousands of other potential customers and lets you post some great reasons why people do need insurance. So, get with an online marketing program and make sure your website (and social media) are geared to educate and protect.
The post Online marketing is going to be with us for decades to come first appeared on SEONewsWire.net.]]>One of the most frequent issues I face revolves around the discharge of a resident from a nursing home. Often times, an agent or advocate visits my office with a concern, because their loved one is being discharged from the nursing home, and they want to assess what their options are. The good news is that the nursing home cannot just kick a resident out of the nursing home.
A common discharge is related to a loss of Medicare coverage for rehab or skilled nursing care. Under Medicare rules, coverage of rehab services will not extend beyond day 100 and will be cut short due to a refusal to participate in therapies or if daily skilled care is no longer necessary. However, what most facilities fail to explain to the residents and their advocates is that they have the option to remain in the facility, and the nursing home may only involuntarily discharge under a set of parameters as set forth under the Nursing Home Reform Act. Specifically, a nursing home must allow a resident to remain in the facility unless one of the following conditions is met:
- the resident’s welfare cannot be met in the facility;
- the resident no longer needs the services provided by the facility;
- the safety of individuals in the facility is endangered;
- the health of individuals in the facility would otherwise be endangered;
- the resident has failed, after reasonable and appropriate notice, to pay for a stay at the facility; or
- the facility ceases to operate.
And, even under those circumstances, the facility is still responsible for the development of a safe-discharge plan. Specifically, a facility is responsible for developing a post-discharge care plan that assesses the continuing care needs and development of a plan designed to ensure the individual’s needs will be met after discharge from the facility into the community.
All too frequently, we receive a statement from a discharge planner that the “safe-discharge plan” includes going to an assisted living facility or returning home with private duty staff to assist with 24/7 care. The problem; however, is that the resident may not be able to afford either of those options, and as a result, would not be safe alternatives to the nursing home. Not only has the nursing facility not informed the resident of his or her right to remain at the facility under private pay (or that Medicaid may be able to assist with paying for care), but has failed to consider whether the “safe-discharge plan” is a viable option.
The question then becomes what is the motivation to discharge a patient. It is simple– the nursing home is a business. Most nursing homes prefer Medicare reimbursement or private pay over Medicaid reimbursement to protect the financial stake of the company. Furthermore, most nursing homes prefer residents who do not have extraneous care needs or advocates that are determined to present a problem to a nursing home.
So, you are probably wondering what you can do in light of an improper discharge:
- Appeal the discharge. If you feel that your loved one still requires skilled nursing care or is otherwise being improperly discharged, you may appeal the decision. The facility is required to provide you with a statement pertaining to your right to appeal with the discharge notice.
- Demand bill. If you disagree with a facility’s decision of coverage, you may request that the facility submit the bill to Medicare even when the facility believes that services will not be covered by Medicare. The facility cannot bill the beneficiary for the disputed charges until the Medicare fiscal intermediary issues a formal claim determination. If the determination is unfavorable, you should be prepared to pay for the expense.
- Find an alternative source for payment. Understand that your loved one’s stay in the nursing home will not be covered by Medicare as of day 101 of institutionalization. If your loved one cannot afford the private pay rate, act promptly to develop a plan for long-term payment in facility. It is imperative that you determine whether an application for Medicaid is necessary, and that the necessary planning for Medicaid, and the submission of an application, occur prior to the expiration of the Medicare covered period.
- Investigate bed certification. Many facilities will inform a resident that they do not have any more Medicaid beds available, despite the fact that most facilities have dually-certified beds. What this means is that if you are currently in a bed, they must allow you to stay in the bed even if you are on Medicaid – the number of “Medicaid beds” is most often determined by the facility itself for budgetary purposes.
- Be Prepared for a Hospital Discharge. A facility may have the resident admitted to a hospital on in-patient status and deny readmission. Since Virginia Medicaid does not pay for a bed hold, you should consider privately paying for a bed hold.
- Do not sign in an individual capacity. If you are an agent for the resident, you should never sign the nursing home admission documents in your personal capacity, and the nursing home cannot require you to sign as a responsible party. Instead, you should clarify, in writing that you are signing on behalf of the resident.
Seek an experienced advocate. If you feel something isn’t right, you should seek someone experienced with resident rights.
 Ask Kit Kat – Helping Feral Cats
Ask Kit Kat – Helping Feral Cats
Hook Law Center: Kit Kat, what can someone do to help feral cats which may be living in a neighborhood?
Kit Kat: Well, there are some things which can be done, but you will need help from your community. At least, that is what is suggested in a recent article in the All Animals magazine published by the Humane Society of the United States (HSUS). In that article, it is suggested that the person spearheading the effort must first talk to their neighbors and get their input. If one person just captures a few cats with traps, there may be many more out there who will continue breeding, and the situation will not become manageable. Let me provide an example, so you will see what I mean.
Beth McNulty, an operations manager with the HSUS, who lives in rural Monrovia, MD noticed in 2010 a spike in the number of stray cats which were wandering through her yard. Occasionally, she would see one or two, but this was almost a dozen. She herself had 3 indoor cats, and one was just recovering from a spraying behavior, so she was afraid to take in anymore cats would set hers off again. In her sleuthing, she discovered that the cats had been living in a nearby junkyard which was being cleaned out. The cats fled in the confusion. To make a long story short, she discovered that the best way to start the process of helping the feral cat colony was to involve her neighbors. Their awareness and help resulted in a neighborhood-wide trapping effort. Thirty older cats and older kittens were sterilized, and returned to their former abode (the now clean junkyard). Three small kittens were placed with a rescue group. McNulty hasn’t seen another addition to the clan yet. This approach of capturing feral cats, sterilizing them, and returning them to live on their own is known as TNR (trap-neuter-return). It appears to be a humane way of caring for them without resorting to euthanasia.
You can tell if a feral cat has been sterilized by a clipped ear lobe. That is done after the sterilization, so all will know. How can you tell the difference between someone’s pet who has just gotten lost or a feral cat? Usually, the feral cat will not eat in the presence of a human. The feral cat will only eat after the human has walked away. So, be aware of stray cats in your community. There may be a way to humanely maintain them there, as they live out their lives.(Julie Falconer, “The Outsiders-How to Help your Neighborhood’s Felines,” All Animals, July/August 2016, p. 16-21)
Distribution of This Newsletter
Hook Law Center encourages you to share this newsletter with anyone who is interested in issues pertaining to the elderly, the disabled and their advocates. The information in this newsletter may be copied and distributed, without charge and without permission, but with appropriate citation to Hook Law Center, P.C. If you are interested in a free subscription to the Hook Law Center News, then please telephone us at 757-399-7506, e-mail us at mail@hooklawcenter.com or fax us at 757-397-1267.The post Understanding a Resident’s Transfer and Discharge Rights under the Nursing Home Reform Act first appeared on SEONewsWire.net.]]>
by Thomas D. Begley, Jr., CELA
A Disability Annuity Trust (“DAT”) can be established for a disabled child or any disabled individual.[1] However, in considering the use of a DAT for a disabled person, care must be taken to examine the other government benefits currently being received, or which may be received in the future by the person with disabilities.
If the person with disabilities is receiving Supplemental Security Disability Income (“SSDI”), this is usually accompanied by Medicare. SSDI and Medicare are insurance-based programs, rather than means-based programs. Receipt of income from the DAT would not cause a loss of SSDI or Medicare. However, consideration should be given to other benefits that the person with disabilities may receive in the future. For example, will the person with disabilities be a candidate for group housing in the future? If so, the existence of the DAT may cause them to lose that benefit.
If the person is receiving Supplemental Security Income (“SSI”), that person also receives Medicaid. SSI is a means-based program. Both resources and income are considered in determining eligibility. If the person with disabilities receives distributions from the DAT, this may well disqualify that person from receiving SSI and cause a loss of Medicaid. The assets in the DAT would be “available” which would also disqualify the SSI recipient from both SSI and Medicaid, because the assets in the trust would be considered resources. If a DAT is designed as a Special Needs Trust, public benefits may be preserved.
[1] HCFA Transmittal 64 § 3257(B)(6).
The post ESTABLISHING A DISABILITY ANNUITY TRUST FOR A BENEFICIARY RECEIVING SSDI OR SSI first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
The Concept. A sole benefit of trust is a creature of HCFA Transmittal 64.[1] These trusts have traditionally been used in crisis planning. They can be established for the benefit of disabled persons—a Disability Annuity Trust (“DAT”).[2] The idea is that assets would be transferred to an irrevocable trust for the sole benefit of the disabled individual. The assets in the trust were then paid out to the beneficiary on an actuarially sound basis using the actuarial tables contained in HCFA Transmittal 64.[3] However, some states, including New Jersey, maintain that despite the clear language in HCFA Transmittal 64, the language in the statute “sole benefit of” means that a Medicaid payback provision is required. Because the assets were transferred to an irrevocable trust “for the sole benefit of” a disabled individual, the transfer is not subject to the Medicaid transfer penalty rules.
This is a particularly useful device where (1) there are highly appreciated assets and utilization of the trust makes it possible for a “step up” in basis to be obtained, and (2) advanced planning has not been done and the transfer of assets to children would result in significant periods of Medicaid ineligibility. There are two issues to be considered in utilizing “for the sole benefit of” trusts: transfer rules and availability.
Transfer of Asset Penalty. A sole benefit of trust is exempt from the Medicaid transfer of asset penalties. If the sole benefit of trust is established for a disabled child, there is no age limit.
Age Limit.
- Sole benefit of disabled child. The trust can be established for a disabled child age 65 or older.[4]
- Sole benefit of other disabled individual. If the sole benefit of trust is established for an individual other than a child, the other individual must be under age 65 years of age and disabled.[5]
Definition of sole benefit of. HCFA Transmittal 64 deals with transfers of assets and treatment of trusts.[6] For the sole benefit of is defined as follows:
A transfer is considered to be for the sole benefit of a spouse, blind or disabled child, or a disabled individual if the transfer is arranged in such a way that no individual or entity except for the spouse, blind or disabled child, or disabled individual can benefit from the assets transferred in any way, whether at the time of the transfer or at any time in the future. For a transfer or trust to be considered for the sole benefit of one of these individuals, the instrument or document must provide for the spending of funds involved for the benefit of the individual on a basis that is actuarially sound based on the life expectancy of the individual involved.[7]
Despite the clear definition of sole benefit of in HCFA Transmittal 64, many states, including New Jersey, require that the sole benefit of trust have a provision requiring a payback on the death of the beneficiary to the state Medicaid agency.
Therefore, if the beneficiary is receiving Social Security Disability Income (“SSDI”) and Medicare, a DAT is appropriate. Beneficiaries receiving Supplemental Security Income (“SSI”) and Medicaid must utilize a Disability Annuity Special Needs Trust.
[1] HCFA Transmittal 64 § 3257.
[2] HCFA Transmittal 64 § 3258.9B.
[3] HCFA Transmittal 64 § 3258.9B.
[4] 42 U.S.C. § l396p(c)(2)(B)(iii).
[5] 42 U.S.C. § l396p(c)(2)(B)(iv).
[6] HCFA Transmittal 64 § 3257.
[7] HCFA Transmittal 64 § 3257(B)(6).
The post DISABILITY ANNUITY TRUSTS first appeared on SEONewsWire.net.]]>by Joyce Frieden
News Editor, MedPage Today
CHICAGO — A proposal by the Centers for Medicare & Medicaid Services (CMS) to change the way Medicare pays for drugs under the Part B program would hurt physician practices, the American Medical Association said at its annual meeting here.
“This is a patient care issue and an access issue,” said Heather Smith, MD, an ob/gyn in Bronx, N.Y., who spoke on behalf of the American Congress of Obstetricians and Gynecologists. “This will impact care of our patients, especially those with ovarian cancer.”
The AMA House of Delegates passed a resolution Wednesday asking that CMS withdraw its proposal and, if that doesn’t happen, that the AMA lobby Congress block the proposal’s implementation. The proposal, if put into place, “would significantly undermine the ability of physician practices to meet the significant administrative and financial burdens associated with the rapidly evolving healthcare environment,” according to the resolution.
The CMS plan would replace the current Medicare reimbursement — the average sales price of the drug plus a 6% add-on fee to cover costs — with a rate of the average sales price plus 2.5%, plus a flat fee of $16.80 per drug per day. The flat fee would be adjusted at the beginning of each year.
For full story go to: http://www.medpagetoday.com/MeetingCoverage/AMA/58630
The post AMA Blasts Medicare Part B Drug Price Plan first appeared on SEONewsWire.net.]]>By Thomas D. Begley, Jr.
WHAT IS A QUALIFIED SETTLEMENT FUND?
468B of the Internal Revenue Code[1] authorizes the establishment of Designated Settlement Funds or Qualified Settlement Funds. These funds are usually collectively referred to as Qualified Settlement Funds (QSFs). These funds are also sometimes called 468B Trusts. The purpose of these funds is to permit a defendant in certain types of litigation to deposit funds into a trust and to receive a full and complete release of liability. The defendant is entitled to a current income tax deduction for the amount paid into the fund at the time the funds are deposited into the trust. This is an exception to the general rule under which the tax deduction is not permitted until the funds are actually disbursed to the plaintiff, which is normally the time in which the plaintiff has received the “economic benefit” of the settlement.
QSFs arose out of class action lawsuits. They can be very useful in personal injury actions and other types of cases where there are multiple plaintiffs. The QSF is usually established prior to trial. The parties agree on a global settlement. The defendant pays that amount into the QSF and the plaintiffs can then take their time in allocating the settlement among themselves and in dealing with various liens, such as Medicaid, Medicare, ERISA, and other liens. The QSF could also be established after a jury award, as long as there is an appeal pending.
A QSF need not be a trust. It may be a fund, account, or trust under state law, or its assets must be otherwise segregated from the transferor’s (or related person’s) other assets.[2] Good practice dictates a written trust agreement. An attorney’s trust account could theoretically serve as a QSF.[3] The problem is that State IOLTA (Interest on Lawyer Trust Accounts) Rules require that income from the attorneys’ trust accounts be paid not to the clients but to State IOLTA funds.
When a QSF is being used for asbestos cases, special rules apply.[4]
ADVANTAGES
There are advantages to both the plaintiff and the defendant in utilizing a 468(b) trust.
 Advantages to the Defendant. Advantages to the defendant utilizing a QSF include the following:
Advantages to the Defendant. Advantages to the defendant utilizing a QSF include the following:
- Defendant Removed from Litigation. Defendants want to be out of the case. By using a QSF a defendant can pay and go. The defendant pays the funds into the QSF and the plaintiffs later deal with liens, allocate the settlement between themselves, determine how much should be lump sum and how much to structure, determine whether any Special Needs Trusts are required, and wait while a guardian is appointed for an incapacitated plaintiff, if required.
- Deduction to Defendant. Defendants and their insurers are able to obtain immediate tax deductions, rather than waiting for “economic performance” to occur.
 Advantages to the Plaintiff. Advantages to the plaintiff utilizing a QSF include the following:
Advantages to the Plaintiff. Advantages to the plaintiff utilizing a QSF include the following:
- Defendant Removed from Allocation of Settlement. Where QSF trusts are used, the defendant leaves to the plaintiff the issue of allocating the settlement among injured parties. This often gives the plaintiff greater flexibility in shaping the settlement. There are often advantages to allocating portions of the settlement to family members other than the injured plaintiff.
- Plaintiff’s Attorneys’ Fees and Costs. When a QSF trust is used, the plaintiff’s counsel can be paid fees immediately from the QSF and litigation expenses can also be paid.
- Income to Plaintiff. The plaintiff will immediately begin to receive income from the settlement held by the QSF trust. Without the trust, the defendant would be holding the money and the plaintiff would not be receiving the benefit of the income.
- Negotiations. Time is no longer a factor in negotiations with Medicare, Medicaid, ERISA, and third-party insurers. Additional time is available to negotiate and satisfy those liens.
- Forms of Distributions. Establishment of a QSF trust gives the plaintiff time to determine how much of the settlement to take as a lump sum and how much, if any, to structure.
- Conflict Resolution Among Related Plaintiffs. A QSF trust gives the plaintiff’s attorney, who may be representing more than one family member, time to resolve conflicts between them. One parent may have abandoned the injured child, for example. The other parent may be the custodial parent providing almost total care. How much does each parent receive?
- Removes Defense Structured Settlement Broker from the Case. The relationship between plaintiff’s structure brokers and defense brokers can be rancorous. If the QSF purchases the structure, the defense broker is effectively removed from consideration.
- Eliminates the Risk of Insolvency. If plaintiffs believe that the defendant or the defendant’s insurer is financially unstable, the QSF can be used as a vehicle into which funds can be immediately transferred.
- International Litigation. QSFs can be used to collect settlements from defendants that are located outside the country and can be used by foreign plaintiffs to collect from defendants located in the country.
- In cases involving a large number of claimants, an administrator of a QSF can obtain a Qualified Protective Order (QPO) that complies with the requirements of HIPAA and allows for limited use of Protected Health Information (PHI). This avoids the necessity of obtaining specific HIPAA releases from each settling claimant. Those releases would otherwise be necessary to negotiate subrogation claims in personal injury cases. A QSF administrator often retains the services of an outside vendor for lien resolution. The vendor may be required to disclose PHI to a number of different parties in order to secure release or payment requirements to settle the claims. The QPO is a good solution. A QPO is defined as an order of the court or of an administrative tribunal or a stipulation by the parties to the litigation or administrative proceeding that prohibits the parties from using or disclosing the PHI for any purpose other than the litigation or proceeding for which the information was requested.[5] The regulation further requires the return to the covered entity or destruction of the PHI at the end of the litigation or proceeding.
- Assists Structuring Attorneys’ Fees. Once settlement proceeds are deposited in an attorney trust account, it is too late for the lawyer to structure his fee. By making the deposit into a QSF, plaintiff’s counsel has time to consider payment options including whether or not to structure his fee.
- Multiple Defendants. A QSF can also be useful in cases involving multiple defendants or where all disputes with a single defendant cannot be resolved at one time. All monies can be held in a QSF until all defendants settle.
DISADVANTAGES
A disadvantage of establishing a QSF is the cost. There are fees for the drafting of the trust document including all of the ancillary services, such as obtaining information and explaining the document to all of the parties, filing fees, administration and trustee fees, and, possibly, CPA fees for preparing tax returns. A QSF may not be warranted in smaller cases.
TYPES OF CLAIMS
Which claims are permitted and which are not are considered in the following sections.
 Permitted Claims. A QSF can be used in claims involving:
Permitted Claims. A QSF can be used in claims involving:
- Tort,[6]
- The Comprehensive Environmental Response, Compensation and Liability Act (CERCLA),[7]
- Breach or contract,[8] or
- Violation of law.[9]
In a Private Letter Ruling,[10] the I.R.S. approved the use of a QSF in connection with a bankruptcy case. In that case, the trust was approved by a confirmation order issued by the U.S. Bankruptcy Court, which had continuing jurisdiction over the trust. The trust was established under the laws of the state to resolve employees’ wrongful discharge claims filed under potential theories of tort, breach of contract, or a violation of law. Further, the discharged employees are not general trade creditors of the debtor, nor do their claims belong to any other class excluded by the regulation. Accordingly, the trust is a QSF. The I.R.S. ruled that the debtor is the transferor.
 Prohibited Claims. QSFs may not be used in cases:
Prohibited Claims. QSFs may not be used in cases:
- Arising from worker’s compensation or self-insured health plan,[11]
- Involving liabilities to refund the purchase price of or repair or replace products sold in the ordinary course of the transferor’s business,[12] or
- Involving the obligation of the transferor to make payments to its general trade creditors[13] and debt holders relating to a bankruptcy case or workout.
INCOME TAX CONSIDERATIONS
There are several income tax issues that must be considered in connection with QSFs.
 Economic Performance. Economic performance shall be deemed to occur as qualified payments are made by the taxpayer, usually the defendant’s insurer, to a Designated Settlement Fund (QSF).[14] This means that the defendant receives an immediate tax deduction upon depositing the funds in the QSF.
Economic Performance. Economic performance shall be deemed to occur as qualified payments are made by the taxpayer, usually the defendant’s insurer, to a Designated Settlement Fund (QSF).[14] This means that the defendant receives an immediate tax deduction upon depositing the funds in the QSF.
 Constructive Receipt. Deposit of the funds in the QSF is not constructive receipt. Because the taxpayer’s receipt of income is subject to substantial limitations, constructive receipt is avoided.[15]
Constructive Receipt. Deposit of the funds in the QSF is not constructive receipt. Because the taxpayer’s receipt of income is subject to substantial limitations, constructive receipt is avoided.[15]
 Taxation of Qualified Settlement Funds. Income earned by the QSF is taxed at a rate equal to the maximum rate in effect for such taxable year for trusts.[16] For 2016, the QSF rate is 39.6 percent.[17] All income is taxed at the same rate, there are no lower brackets. The tax is based not on gross income, but on modified taxable income.
Taxation of Qualified Settlement Funds. Income earned by the QSF is taxed at a rate equal to the maximum rate in effect for such taxable year for trusts.[16] For 2016, the QSF rate is 39.6 percent.[17] All income is taxed at the same rate, there are no lower brackets. The tax is based not on gross income, but on modified taxable income.
The 3.8 percent Medicare tax on unearned income also applies.[18] The tax is the lesser of the undistributed net investment income for such taxable year, or the excess (if any) of:[19]
- The adjusted gross income for such taxable year over.
- The dollar amount of which the highest tax bracket begins for such taxable year.
Because QSFs are separate tax entities and pay tax on any interest and dividend income, the after-tax income then becomes part of the settlement fund and distributions to the claimants can be made with after-tax dollars.
 Attorneys’ Fees.
Attorneys’ Fees.
- Plaintiff’s Attorney’s Fees. In most instances, the transferor will transfer to the QSF the entire settlement amount, including that portion that is payable to the personal injury attorney or attorneys for attorneys’ fees under the engagement letters signed between the plaintiffs and plaintiffs’ attorney. In rare instances, the transferor will pay the plaintiff’s attorneys’ fees directly and only transfer to the QSF the net amount due to the plaintiff. When attorneys’ fees are paid to the QSF, they do not represent gross income to the QSF, and when they are paid by the QSF they do not represent a tax deduction to the QSF. The QSF administrator/trustee must determine whether disbursements are subject to withholding requirements and whether disbursements of attorneys’ fees to class counsel in the underlying litigation are reportable.[20]
- QSF Attorneys’ Fees. Normally, a QSF will engage a law firm to perform legal services on behalf of the QSF. Such legal expenses are necessary to administer the QSF and to process claims and are deductible by the QSF as ordinary business expenses.[21] Whether or not the legal fee is immediately deductible or must be capitalized is determined by the origin of the claim.
THE 468B TRUSTEE/TRUST ADMINISTRATOR
The Regulations require that a QSF have an “Administrator.”[22] Unless the QSF is a trust, it is not required to have a trustee. If the QSF is a trust, the same person can serve as both Trustee and Administrator or there can be a separate trustee and a separate Administrator. Generally, the Trustee/Administrator is selected by the plaintiff’s attorney. If there is a separate Trustee and Administrator, the duties of each must be clearly defined in the trust document.
In some instances, a court will require an individual trustee to be bonded, which may be difficult or even impossible. A solution is to appoint the individual as Trust Administrator and appoint a Corporate Trustee. The trust document can give the Administrator the duty to make disbursements subject to court order. The Corporate Trustee would take the QSF deposit, subject to the court order, preventing any release of the funds without prior court approval. A similar result might be achieved by having an individual serve as Trustee/Administrator subject to a “safekeeping agreement” with a cooperating bank. The bank would accept the QSF deposits under court order preventing funds from being released without prior court approval.
DISTRIBUTIONS
The Trustee/Administrator is responsible for making distributions from the QSF to claimants, claimants’ attorneys, State Medicaid Agencies to satisfy liens, CMS to satisfy Medicare liens, ERISA Plans to satisfy ERISA liens, and any other lien holders that require satisfaction from the settlement fund.
STRUCTURED SETTLEMENTS
The Trustee/Administrator will be responsible for arranging structured settlements, including making a § 130 Qualified Assignment to a third-party assignee who will make the periodic payments.
[1] I.R.C. § 468B.
[2] Treas. Reg. § 1.468B-1(c)(3).
[3] P.L.R. 200216013 (Jan. 16, 2002).
[4] I.R.S. § 524b.
[5] 45 C.F.R. § 164.512(e)(1)(i).
[6] Treas. Reg. § 1.468B-1(c)(2)(ii).
[7] Treas. Reg. § 1.468B-1(c)(2)(i); 42 U.S.C. § 103.
[8] Treas. Reg. § 1.468B-1(c)(2)(ii).
[9] Treas. Reg. § 1.468B-1(c)(2)(ii).
[10] Priv. Ltr. Rul. 14-90-64-(2005).
[11] Treas. Reg. § 1.468B(1)(g)(3)(1).
[12] Treas. Reg. § 1.468B(1)(g)(3)(2).
[13] Treas. Reg. § 1.468B(1)(g)(3)(3).
[14] I.R.C. § 468B(a).
[15] Treas. Reg. § 1.451-2.
[16] I.R.C. § 468B(b)(1) and I.R.C. § 1(e).
[17] I.R.C. § 411(b).
[18] I.R.C. § 1411(a)(2).
[19] I.R.C. § 1411(a)(2).
[20] I.R.C. § 6041.
[21] Treas. Reg. § 1.468B-2(b)(2).
[22] Treas. Reg. § 1.468B-2(k)(3).
The post Qualified Settlement Funds first appeared on SEONewsWire.net.]]>Medicare
Medicare only covers care that is medically necessary, including medical acute care, such as visits to the doctor, medications and time spent in the hospital. In addition, Medicare covers short-term services for ailments that are predicted to improve, including physical therapy.
In order to become eligible for Medicare, you must be age 65 or older, under age 65 with certain disabilities, or any age and have end-stage renal disease, which is permanent kidney failure that has to be treated with dialysis or a kidney transplant.
Medicare does not pay for the most significant aspect of long-term care services or personal care, including assistance with bathing, or for supervision that is frequently referred to as custodial care. Medicare covers the cost of a brief stay in a skilled nursing facility, hospice care, or home health care if you meet certain conditions:
You have recently stayed in a hospital for a minimum of three days;
Within 30 days of your time previously spent in a hospital, you were admitted to a nursing facility that is certified by Medicare;
You require skilled care, including skilled nursing services, physical therapy or other kinds of therapy.
If you meet each of these conditions, Medicare will pay for some of the expenses for a maximum of 100 days. For the initial 20 days, Medicare pays 100 percent of your expenses. Then you are responsible for your expenses up to $140 per day, as of 2013. Medicare pays any remaining balance. After day 100, you are responsible for the entire cost of each day spent in a skilled nursing facility.
Medicare also pays for specific long-term care services for a certain period of time if your physician states that they are medically needed to treat an illness or injury. If you suffer from a terminal illness, and it is anticipated that you will not live more than six months, Medicare will pay for hospice care.
Medicaid
Medicaid is a joint federal and state government program that assists low-income people with the payment of part, or all, of their health care expenses. It covers medical care, including visits to the doctor, and the cost of hospital stays. It also covers long-term care services in nursing homes, as well as those given at home, including visiting nurses and help with personal care. Medicaid differs from Medicare in that it covers the cost of custodial care in nursing homes and at home.
In order to become eligible for Medicaid, you must meet certain qualifications, including having earnings and assets that are not greater than the levels used by your state. Under federal law, if Medicaid pays for your long-term care services, that state must recover the amount that Medicaid expended on your behalf from your estate after your death. This is called Medicaid Estate Recovery.
The elder law attorneys at Hook Law Center assist Virginia families with will preparation, trust & estate administration, guardianships and conservatorships, long-term care planning, special needs planning, veterans benefits, and more. To learn more, visit http://www.hooklawcenter.com/ or call 757-399-7506.
The post Learn what government benefits are available to help pay for long-term care first appeared on SEONewsWire.net.]]>by Melanie S. Kaplan, Esquire
As of July 1, 2014, what was formerly known as Global Options for Long Term Care (GO) is now known as Managed Long Term Services and Supports. (MLTSS). Individuals previously receiving benefits under AIDS Community Care Alternatives Program (ACCAP), Community Resources for People with Disabilities (CRPD) and Traumatic Brain Injury (TBI) were automatically enrolled in the MLTSS program. The MLTSS program was designed to permit individuals to live in the community for as long as possible with services and support.
The change from GO to the MLTSS program has reduced the number of programs and service providers and has simplified the services provided. There are no longer enrollment caps and waiting lists for community and home based services, as existed under the above mentioned waiver programs.
The MLTSS program is for individuals who require services and support that are living at home, in an assisted living facility, in community residential services, as well as those in a nursing home. MLTSS participants must meet income and asset requirements, as well as be determined clinically eligible. An MLTSS participant must meet a nursing home level of care, which means that she or he requires limited assistance with a minimum of 3 activities of daily living (ADL) or the individual has cognitive deficits and requires assistance with more than 3 ADL areas. MLTSS strives to assist participants to live as independently as possible for as long as possible while focusing on the individual’s care needs.
A care manager will work with each individual to create a plan specific to their needs. The care manager will create a Plan of Care, as well as assist in selecting and arranging such services and ensuring that all medical visits take place. With the help of the care manager, the participant is able to determine which services he or she needs, select providers of the needed services and ensure that those services are in fact implemented.
Eligibility
To be eligible for MLTSS, an individual must meet all of the following criteria:
➢ Resident of New Jersey
➢ 65 years of age or older, or under age 65 and determined to be blind or disabled under the Social Security Administration or the Division of Medical Assistance and Health Services
➢ Qualify for Medicaid financially, this includes monthly income, as well as total liquid assets
- Income for a single applicant can be equal to or less than $2,199 per month (2016).
- Income for a couple, who are both applying, can be equal to or less than $4,398 per month (2016).
- If an individual’s income exceeds $2,199.00 then a Miller Trust, also known as a Qualified Income Trust (QIT) will be required.
- Resources must be at or below $2,000 for an individual and $3,000 for a couple, where both individuals are applying for services.
- Couples, where only one spouse is applying, may keep up to $119,220 in assets, known as the community spouse resource allowance (CSRA). (2016)
➢ Clinically eligible for a nursing home level of care, meaning that the individual requires assistance with activities of daily living. A clinical assessment will be performed before an individual enters the MLTSS program.
Services
The MLTSS program uses NJ Family Care managed care organizations to coordinate all services provided under the program. Each participant is provided with an individualized Plan of Care (POC). This assessment is continually reviewed and updated at least annually.
Description of Services Provided
MLTSS services include the following:
➢ Personal Care;
➢ Respite;
➢ Care Management;
➢ Home and Vehicle Modifications;
➢ Home Delivered Meals;
➢ Personal Emergency Response Systems;
➢ Mental Health and Addiction Services;
➢ Assisted Living;
➢ Community Residential Services;
➢ Nursing Home Care.
➢ Transportation
Description of Service Providers
Managed Care Organization (MCO)
Under a MCO an individual will need to enroll in one of the following:
➢ Amerigroup New Jersey, Inc.
➢ Aetna Better Health of NJ
➢ Horizon NJ Health
➢ UnitedHealth Care Community Plan
➢ WellCare Health Plans of New Jersey
Program of All-Inclusive Care for the Elderly (PACE)
Individuals entering a Nursing Home for the first time will have their primary health care managed by NJ Family Care with MLTSS or the Program of All-Inclusive Care for the Elderly, known as the PACE program. To be eligible for the PACE program, the individual must live in a PACE service area. There are currently five PACE organizations in eight counties in New Jersey.
➢ LIFE (Living Independently for Elders) St. Francis, operated by St. Francis Medical Center. This program services Mercer County and Burlington County.
➢ LIFE at Lourdes operated by Our Lady of Lourdes Medical Center. This program services most of Camden County.
➢ Lutheran Senior LIFE located at Jersey City Medical Center. This program services most of Hudson County.
➢ Inspira LIFE, operated by Inspira Health Network. This program services portions of Cumberland County, Gloucester County and Salem County.
➢ Beacon of LIFE, located in Oceanport. This program services most of Monmouth County
To be eligible for PACE, an individual must meet all of the following criteria:
➢ An individual must be age 55 or older
➢ The individual must be in need of a nursing home level of care, but able to live in the community
➢ The individual must reside in a PACE service area.
The PACE program is a Medicare program that provides individuals with medical and social services in order to assist those individuals in delaying long-term nursing home care. PACE participants receive a customized plan of care that is reevaluated on a regular basis.
Through the PACE program, an individual receives the same services provided by Medicare and Medicaid, without the same limitations. PACE may also provide additional services determined to be necessary for a particular individual, in order to help keep that individual in the community. PACE services include, but are not limited to:
➢ Primary care
➢ Prescription drugs
➢ Adult day care
➢ Home and personal care services
➢ Nutrition services
➢ Transportation
➢ Hospital care
➢ Nursing home care
PACE organizations receive funding from Medicare and Medicaid each month. Participants of the PACE program may elect to disenroll from the program at any time and return to their former health care coverage.
Cost Share
The county welfare agency will determine the cost share for individuals residing in a facility. The cost share will be based on his or her monthly income.
Disenrollment
MLTSS is a voluntary program so participants can withdraw at any time. Alternately, a participant may be disenrolled for a variety of reasons, including if he or she no longer meets the financial or clinical eligibility criteria or if he or she moves out of New Jersey.
Recourse
An MLTSS participant has the right to request a fair hearing provided by the Office of Administrative Law if he or she is determined ineligible or denied services, or if services are suspended, reduced, or terminated. The state will provide 30 days’ notice of termination of benefits unless the reason for disenrollment is that the participant has moved out of the state. Once provided written notice of the action, the participant must request a fair hearing within 20 days of the date of the letter. Medicaid benefits may continue until a hearing decision is reached; however, if the hearing decision is not in the participant’s favor, the participant may be required to repay the cost of benefits that he or she was not entitled to receive.
The post MEDICAID MANAGED LONG-TERM SERVICES AND SUPPORTS first appeared on SEONewsWire.net.]]>Before you buy leads you need to ask yourself a lot of questions. This helps you focus what you want in terms of leads, leads with the potential to convert and build your business. If you sell final expense insurance or term insurance you do not want leads for group insurance. It’s all about knowing your market niche and making plans to work it smart.
What do you need to know before you call to order leads? Some of the questions you should write down before you call and interview the lead company you want to work with are: Where do you get your leads from, how old are the leads, are they guaranteed to be accurate and do you have the time to follow up the leads in a timely and consistent manner?
Where a lead generation company gets its leads to sell to you is a very important question for this reason, the best sources are those that have specifically expressed an interest in the type of insurance you sell – say Medicare or long-term disability. These exclusive leads may be more expensive, but they have a higher conversion rate.
Make sure you do not get really old leads, which fall into the category of “cold” leads. There are several issues with old leads, not the least of which is the information may no longer be accurate, the individual(s) may not even recall requesting information and they may no longer be interested. Buying old, cold leads is a waste of time and money, even if they are inexpensive. These leads are usually sold and resold to multiple agents and the only one that makes money in that deal is the lead generation company.
If you choose to buy exclusive leads, then ask if the lead generation company has a guarantee about their accuracy. Some companies do replace any leads that are not accurate. Since it is your marketing dollars being spent on exclusive leads, you want to know any duds will be replaced.
Having said all that, make sure you have the time to follow up your leads. If you do not consistently follow up you run the risk of losing potential customers. Your business needs a continuous source of customers to grow. Do it the right way the first time.
The post Buy the Right Kinds of Leads Specific to Type of Insurance Sold first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
For many years a debate has raged as to whether Medicare’s interests must be considered with respect to future medical payments in the context of a third party liability settlement (“TPLS”). The issue is simple. If a plaintiff in a TPLS receives money to pay for future medical care, is he free to pocket that money and send the bill for the future medical care to Medicare? Under the Medicare Secondary Payer Act (“MSPA”), Medicare is prohibited from making a payment for future medicals to the extent that such payment has been made under liability insurance. Therefore, if a liability insurance company or self-insured defendant pays money to a plaintiff for future medical care, the argument goes that Medicare cannot pay for that care.
In 2013, the Centers for Medicare and Medicaid Services (“CMS”) issued a Notice of Proposed Rulemaking (“NPRM”), but then voluntarily withdrew it in 2014. As a result, parties have been left to their own devices in determining how to address this issue. Some commentators believe that absent enforceable regulations that identify the standards by which future medicals are to be measured in the liability context, the federal government has no right to claim an interest in future medicals as part of the settlement. On the opposite end of the spectrum, commentators observe that CMS interprets the MSPA so that it is applicable to TPLS as well as Worker’s Compensation claims. The correct position may lie somewhere in between. The real answer may be to develop an analysis of how much of the TPLS was for future medicals and how much for other elements of damages and to set the future medical money aside, so that Medicare is not billed until that portion of the settlement is exhausted.
Once a Medicare Set-Aside Arrangement (“MSA”) has been considered, the next question is how much is necessary to fund it. If future medicals have been plead or claimed and future medicals are specifically released in a Release signed in connection with the third party liability (“TPL”) settlement, then it is likely that Medicare’s interests must be considered. That raises the question as to how to calculate the amount of the settlement intended for future medical care. It is unlikely that CMS would accept a figure agreed upon by the parties absent court testimony and a court finding.
It is important to remember that in a TPL case, the award seldom pays 100 cents on the dollar for future medicals. Issues in these cases, such as disputed liability or causation, policy limits, statutory caps and derivative claims, often mean that TPL cases are resolved for less than the full measure of damages sustained. The Garretson Resolution Group recommends a starting point for a maximum amount may be identified through review of a plaintiff’s life care plan and other evidence of the dollar assigned to particular damages other than future medicals. These would include procurement costs, liens, past medicals, pain and suffering, loss of future earning capacity, etc. Garretson outlines a four-step process:
- Were future medicals plead or released as part of the settlement, judgment or award?
- Does the plaintiff require future injury-related care?
- Does the settlement award “compensate” plaintiff for future medicals based on objective decisional future medical allocation methodology?
- How much did the settlement award compensate based on objective decisional future medical allocation methodology?
By analyzing the settlement to figure out how much would be appropriate for future medicals and then determining the ratio of the plaintiff’s net proceeds to the total damages, a percentage for future medicals can be determined. This is the amount “compensated” for future medicals within the settlement or award. This would only be the amount necessary to set aside to satisfy CMS.
This approach is different from the traditional approach. The traditional approach to funding an MSA is to determine what the future medical costs to be paid by Medicare would be and set that money aside without regard to whether the plaintiff actually recovered that amount for future medicals. Under the Garretson approach, the only amount to be set aside would be the actual funds recovered by the plaintiff, which could be considerably less than the total future medicals.
Once the amount of the MSA has been determined, who shall administer those funds? One option is to use a professional custodian such as Medi-Vest. The advantage to the professional custodian is that they know the rules. They use the set-aside funds only to pay for medical care that Medicare would cover. The plaintiff may be receiving other medical care that would not be covered by Medicare and use of the MSA funds for payment of that care would be inappropriate. A professional custodian will also take advantage of the discounts offered to Medicare, rather than paying full retain prices. This makes the funds last longer. The other option is to turn over the MSA amount to the plaintiff to be self-administered. The advantage to this approach is that it avoids paying the professional custodian’s fees. There is usually a set-up fee and an annual maintenance fee. A disadvantage to a self-administered MSA is the plaintiff does not know the rules and often uses the funds for other purposes such as covering delinquent mortgage payments or payments on car loans. As a practical matter, if the Set-Aside is a $100,000 or more, it usually makes sense to engage the services of a professional custodian. If the settlement is less than $100,000, the cost of a professional custodian are not warranted and a self-administered MSA is more appropriate.
The next consideration for an MSA is whether or not a Structured Settlement should be considered. CMS requires that an MSA be funded with a lump sum sufficient to cover two year’s medicals plus the first surgery, but the rest can be funded with a Structured Settlement. Since most of the funds will not be needed right away, it often makes sense to use the Structured Settlement. Statistics show that where a Structured Settlement is used, the cost is only 52% of funding an MSA with a lump sum. This is because the Structure does not have to pay out for a period of time. The Structure can also take advantage of the plaintiff’s rated age.
The post DO WE STILL NEED TO WORRY ABOUT MEDICARE SET-ASIDE ARRANGEMENTS? first appeared on SEONewsWire.net.]]>
Many seniors are at risk of falling victim to con artists who prey on them in an effort to gain access to their savings and any assets they have accumulated over the years. An example of such a scam occurs when a fraudulent individual pretending to be an IRS agent telephones the potential victim, stating that the individual owes unpaid back taxes, and makes threats to sue or arrest the senior, or suspend their driver’s license.
Seniors are also susceptible to health care scams in which people call posing as health care or Medicare representatives in an attempt to obtain the senior’s personal and contact information. They will then call the senior back at some future date, stating that they communicated with their son or daughter, who said it was fine to give them their Social Security number. In addition, scammers may offer to help seniors obtain health insurance. The National Council on Aging said that in several cases, they use the personal information to bill Medicare, and keep the funds.
Seniors must also exercise caution when dealing with professionals in whom they have placed their trust, such as financial advisers. It is not unheard of for such advisers to commit fraud and embezzle funds from seniors’ investment accounts. For this reason, it is important to use only established firms as advisers.
Some con artists will even go so far as to pose as a grandchild or great-grandchild in an attempt to secure funds from the senior. In addition, due to the increasing cost of prescription drugs, some seniors search for drugs online. But many of these drugs are counterfeit. Or, upon receipt of funds, the scammers just accept the money without delivering the medications.
Another scam is the obituary scam in which the con artist reads the obituaries, and contacts the family members to inform them that the deceased left an outstanding debt, and is calling to collect on the debt.
Fraudulent behavior has also been committed by people who work at funeral homes. They will advise the senior to purchase the priciest casket, even when a cremation will be performed. They may also add extra charges to the bill for cemetery plots.
Furthermore, tech support scams occur in which a person calls the senior pretending to be a technician from Microsoft or another well-known brand. The person then uses scare tactics to say that there is a virus on the computer and the technician must remotely access the computer in order to install software. Then the scammer requests payment in the form of hundreds of dollars via online or with the use of a credit card, and if the senior resists, the scammer threatens to destroy the computer.
Consumers can report scams to the Federal Trade Commission by calling 1-877-FTC-HELP or visiting ftc.org/complaint.
The post Beware of Scams Targeting the Elderly first appeared on SEONewsWire.net.]]>The thing to remember when calling leads is that you are running a business and in order to keep running it successfully, you need to make your calls and convert those leads. Leaving hot leads in your mailbox for a couple of days diminishes the chances of a sale and increases the chances that the prospective customer thinks no one is going to call.
You need to be very organized when you prepare to make calls to insurance leads. Have everything right at your fingertips: your script, any sales literature pertaining to special policies, Medicare information if you specialize in Medical supplements, information on the latest trends in the insurance market that may affect a consumer, a ready smile and a drive to succeed. Yes, you do smile when you are on the phone. It’s infectious and can be hear by your potential customer.
Everyone has bad days, but leave those angry feelings at home or at the door of your business before you pick up the phone to call. You are marketing yourself, and you want to do it the right way. You must know your policies inside out, how they can be adapted to buyer’s needs, what carriers can do special exceptions for a potential customer, and how you can make your lead’s life a lot easier and safer with the right insurance policy.
The more you work on your selling skills the better you get at selling insurance. It just takes the will, drive and dedication to make it all come together and build your business.
The post Summing it all up to sell insurance first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
Once a Medicare Set-Aside Arrangement (“MSA”) has been considered, the next question is how much is necessary to fund it. If future medicals have been plead or claimed and future medicals are specifically released in a Release signed in connection with the third party liability (“TPL”) settlement, then it is likely that Medicare’s interests must be considered. That raises the question as to how to calculate the amount of the settlement intended for future medical care. It is unlikely that the Centers for Medicare and Medicaid Services (“CMS”) would accept a figure agreed upon by the parties absent court testimony and a court finding.
It is important to remember that in a TPL case, the award seldom pays 100 cents on the dollar for future medicals. Issues in these cases, such as disputed liability or causation, policy limits, statutory caps and derivative claims, often mean that TPL cases are resolved for less than the full measure of damages sustained. The Garretson Resolution Group recommends a starting point for a maximum amount may be identified through review of a plaintiff’s life care plan and other evidence of the dollar assigned to particular damages other than future medicals. These would include procurement costs, liens, pain and suffering, loss of future earning capacity, etc. Garretson outlines a four-step process:
- Were future medicals plead or released as part of the settlement, judgment or award?
- Does the plaintiff require future injury-related care?
- Does the settlement award “compensate” plaintiff for future medicals based on objective decisional future medical allocation methodology?
- How much did the settlement award compensate based on objective decisional future medical allocation methodology?
By analyzing the settlement to figure out how much would be appropriate for future medicals and then determining the ratio of the plaintiff’s net proceeds to the total damages, a percentage for future medicals can be determined. This is the amount “compensated” for future medicals within the settlement or award. This would only be the amount necessary to set aside to satisfy CMS.
This approach is different from the traditional approach. The traditional approach to funding an MSA is to determine what the future medical costs to be paid by Medicare would be and set that money aside without regard to whether the plaintiff actually recovered that amount for future medicals. Under the Garretson approach, the only amount to be set aside would be the actual funds recovered by the plaintiff, which could be considerably less than the total future medicals.
The post HOW MUCH MUST BE SET ASIDE FOR MEDICARE IN A THIRD PARTY LIABILITY CASE? first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
For many years a debate has raged as to whether Medicare’s interests must be considered with respect to future medical payments in the context of a third party liability settlement (“TPLS”). The issue is simple. If a plaintiff in a TPLS receives money to pay for future medical care, is he free to pocket that money and send the bill for the future medical care to Medicare? Under the Medicare Secondary Payer Act (“MSPA”), Medicare is prohibited from making a payment for future medicals to the extent that such payment has been made under liability insurance. Therefore, if a liability insurance company or self-insured defendant pays money to a plaintiff for future medical care, the argument goes that Medicare cannot pay for that care.
In 2013, the Centers for Medicare and Medicaid Services (“CMS”) issued a Notice of Proposed Rulemaking (“NPRM”), but then voluntarily withdrew it in 2014. As a result, parties have been left to their own devices in determining how to address this issue. Some commentators believe that absent enforceable regulations that identify the standards by which future medicals are to be measured in the liability context, the federal government has no right to claim an interest in future medicals as part of the settlement. On the opposite end of the spectrum, commentators observe that CMS interprets the MSPA so that it is applicable to TPLS as well as Worker’s Compensation claims. The correct position may lie somewhere in between. The real answer may be to develop an analysis of how much of the TPLS was for future medicals and how much was for other elements of damages. Then set aside only the amount received for future medicals, not the total anticipated costs of what the future medicals will actually be.
The post DO WE STILL NEED TO WORRY ABOUT MEDICARE SET-ASIDE ARRANGEMENTS? first appeared on SEONewsWire.net.]]>

In Withers v. City of Detroit, the Michigan Court of Appeals reversed a lower court ruling that would have allowed the case to proceed.
According to court records, the question was whether plaintiff had properly notified the city of the potential for a tort claim after she fell into the hole. Plaintiff sent her notice through regular mail (when it should have been certified) to the city’s law department (when it should have gone to the city mayor, clerk or city attorney).
But this did not comply with state statutes in Michigan, which require notice of any injury sustained by reason of a defective highway must be served on an individual – personally or by certified mail, with return service requested – who may be lawfully served with civil processes on behalf of the agency.
Plaintiff didn’t do this. Thus, the appeals court ruled, her claim could not be allowed to proceed.
The letter she had sent was in October 2013. The letter indicated she suffered bodily injury after falling into an uncovered manhole, shortly before 6 a.m. She indicated she was driving a bus for Safeway Transportation, a contractor of the city’s school system. An accident occurred nearby, and plaintiff stepped out to survey it. As she stepped out of the bus, she fell into a manhole that was not covered. As a result, she suffered a serious injury that included five fractures and was unable to work for months.
Soon after, plaintiff mailed her Medicare forms to the office, describing the injuries in more detail.
About four months later, she filed a personal injury lawsuit against the city, alleging the local government negligently failed in its duty to cover that manhole.
Defendant responded with a motion for summary judgment, arguing the notice plaintiff gave was insufficient and failed to conform to state statute regarding government notice of claims. First, the city noted it hadn’t properly received notice of the lawsuit (in the wrong manner to the wrong people), which had to happen before the lawsuit was filed. Further, plaintiff never in her complaint specifically identified the manhole covers or detailed her injuries in depth.
By that time, it would have been too late for plaintiff to refile that notice, as it had to be done within 120 days of the time of injury.
Florida courts have similar rules about proper notice with regard to government claims. F.S. 768.28 details Florida’s waiver of sovereign immunity in tort actions. No lawsuit can be filed until the person first files a notice of claim with the appropriate agency. Further, while personal injury claims are normally four years, claims against the government have to be filed within three years. The lawsuit can only be filed after the appropriate government agency has been notified, given 180 days to conduct a full investigation of the claim and issues a denial of the claim.
Failure to follow this strict procedural requirements can result in dismissal of the claim, as the Withers case shows.
If you have been a victim of a traffic accident, call Chalik & Chalik at (954) 476-1000 or 1 (800) 873-9040.
Additional Resources:
Withers v. City of Detroit, Feb. 18, 2016, Michigan Court of Appeals
More Blog Entries:
Parents: Car Death of Teen Ejected From Fair Preventable, Feb. 23, 2016, Miami Personal Injury Attorney Blog
The post Withers v. City of Detroit – Procedural Problems Plague Injury Case first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
Personal Injury attorneys must inquire as to whether their clients are receiving public benefits. Certain benefits are means-tested, so that if the client receives money directly those benefits are reduced or lost completely. This article will outline the common public benefits and indicate whether the receipt of a personal injury settlement will affect those benefits.
Supplemental Security Income
Supplement Security Income (SSI) is a means-tested federal program that provides income (a cash assistance grant) to certain aged (65 or over), blind, and persons with disabilities. The program is administered by the Social Security Administration. It is governed by federal statute,[1] federal regulations,[2] and the Program Operating Manual System of the Social Security Administration (POMS). For 2016, the maximum federal SSI benefit is $733 per month. In addition, the State of New Jersey has a supplement in the amount of $31.25 per month. If an individual has more than $2,000 of assets, he or she will lose SSI. Therefore, the receipt of a personal injury settlement will disqualify the plaintiff from SSI, unless the funds are placed in a Special Needs Trust.
Social Security Disability Income
This program is known as Old Age Survivors and Disability Insurance (OASDI). It is governed by the Social Security Act.[3] Unlike SSI, which is a means-tested welfare program, Social Security Disability Income (SSDI) is an insurance program. Coverage is based on quarters of Social Security insurance coverage during the applicant’s employment. Receipt of a personal injury settlement will not affect the plaintiff’s SSDI.
Medicaid
Medicaid is a medical insurance program that benefits millions of Americans. There are many ways that individuals qualify for Medicaid. The vast majority of Medicaid recipients receive that benefit, because they are also receiving SSI. If they lose their SSI, they also lose their Medicaid. However, since the Affordable Care Act (ACA), millions of Americans now receive Medicaid regardless of whether or not they are disabled and regardless of whether they are receiving SSI.
For SSI-based Medicaid, there is an asset limit of $2,000. For ACA Medicaid, there is no resource limit. Therefore, receipt of a personal injury settlement by an SSI recipient will cause a loss of Medicaid. However, receipt of a personal injury settlement by a Medicaid recipient who obtained Medicaid through the ACA will not affect eligibility, except that the income from the settlement may push the income of the plaintiff above the income limits for eligibility under the ACA. The solution for an individual receiving SSI-linked Medicaid is a Special Needs Trust. However, under the ACA, only individuals with disabilities are qualified for a Special Needs Trust. Individuals receiving Medicaid under the ACA who are not disabled may not utilize a Special Needs Trust.
Medicaid Waiver Programs
Medicaid Waiver Programs are designed to provide Medicaid coverage for long-term care services. These services are typically delivered in the home or assisted living facilities. These services are vital to catastrophically-injured individuals. These programs have an asset maximum of $2,000. Receipt of a personal injury settlement would disqualify the plaintiff from Medicaid Waiver services, unless the funds are placed in a Special Needs Trust.
Medicare
Medicare is a program that pays medical costs of eligible beneficiaries. Unlike Medicaid, which is a welfare program, Medicare is an insurance program. Receipt of a personal injury settlement will not affect Medicare eligibility.
Federally Assisted Housing
The federal government has two housing programs that provide assistance for low-income individuals and people with disabilities. These are known as Section 2.02 and Section 8. Section 8 is the program that has the most effect on personal injury plaintiffs. The Department of Housing and Urban Development (HUD) pays rental subsidies so eligible families can afford decent, safe and sanitary housing. Each section of the country has a maximum income limit for eligibility for public housing. If a tenant is eligible, they pay 30% of their net income for rent. While there is no asset test for federally assisted housing, if the assets produce income, the income may render the plaintiff ineligible or cause an increase in monthly rental. Income for the entire household is considered.
Payments from a Special Needs Trust are not counted as income, so long as the payments are irregular and sporadic.
Supplemental Nutritional Assistance Program
The Supplemental Nutritional Assistance Program (SNAP) is now the name for a program that used to be called Food Stamps. Recipients are provided an electronic benefit transfer (EBT) card that looks much like a credit card. SNAP eligibility is determined on the basis of household eligibility.
In New Jersey SNAP has complex resource and income limits. Therefore, receipt of a personal injury settlement could disqualify the individual from these benefits, unless the personal injury proceeds are placed in the Special Needs Trust.
Division of Developmental Disability
Many Division of Developmental Disability (DDD) programs are now based on Medicaid eligibility. The asset limit is $2,000. If the plaintiff is receiving or would otherwise be eligible to receive those benefits, then receipt of a personal injury settlement would disqualify them unless it has been placed into a Special Needs Trust. Other DDD benefits would be unaffected by receipt of a personal injury recovery.
Group Home
In New Jersey most group homes are paid with Medicaid dollars. The asset limit is $2,000. Therefore, receipt of a personal injury settlement would disqualify the individual from those benefits, unless it is placed in a Special Needs Trust.
Psychiatric Institutions
Many psychiatric institutions are paid for by Medicaid dollars under Medicaid Waiver Programs. Again, the asset limit is $2,000, so receipt of a personal injury settlement would disqualify the plaintiff unless the funds are placed in a Special Needs Trust.
[1] 42 U.S.C. §1381 et seq.
[2] 20 C.F.R. §416.
[3] 42 U.S.C. §401 et seq. The Regulations are found at 20 C.F.R. §404.1 et seq.
The post PUBLIC BENEFITS CONSIDERATIONS IN PERSONAL INJURY CASES first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., Esquire, CELA
-
- INTRODUCTION
Statistics show that approximately 70% of the population age 65 or over will require some form of long-term care. Some will be there for relatively short periods of time. These are usually stroke victims who are doing rehabilitation. A significant percentage will remain in a nursing home for an extended period of time. These are usually Alzheimer’s or Parkinson’s patients.
A statistic widely quoted is that the average stay in a nursing home is 2.9 years. This statistic is somewhat misleading, because the persons receiving rehabilitation are often discharged in one month or less. The long-term patients may stay in the nursing home for many years.
Unfortunately, as the population ages, the cost of health care is increasing, and government entitlement programs are being cut back. The cost of a nursing home in New Jersey today is approximately $125,000 – $160,000 per year. Some nursing homes are slightly less, and some are significantly more.
There are five sources for nursing home payment. They are: private pay, long-term care insurance, Medicaid, Medicare, and Veterans Administration.
- MEDICAID
2.1. Administration
This is a program administered by the states and funded by both federal and state governments. Rules vary from state to state. In New Jersey, Medicaid is administered by the County Welfare Boards. Medicaid pays for nursing home care for eligible individuals.
2.2. Eligibility
2.2.1. Citizenship and Residency
Must be a U.S. Citizen or resident alien and a resident of New Jersey.[1] An individual is not allowed to enter New Jersey solely in order to receive Medicaid.[2]
2.2.2. Categorical
Must be 65 years of age or older[3] unless blind or disabled.[4] “Blindness” means visual acuity of 20/200 or less in the better eye with use of a correcting lens.[5] “Disability” is defined as the inability to engage in any substantial gainful activity by reason of a medically determinable physical or mental impairment, which can be expected to result in death, or which has lasted or can be expected to last for a continuous period of not less than 12 months.[6]
2.2.3. Medical Eligibility
Must also be eligible from a medical standpoint. This is done by a Medicaid nurse completing a necessary form stating the diagnosis, medication, etc.
2.2.4. Income
2.2.4.1. Cap
New Jersey is an income cap state. This means that if an individual’s income exceeds $2,199 for 2016 (300% of the SSI individual benefit), the individual is not eligible for Medicaid. The solution is to establish a “Miller Trust.” By utilizing the Miller Trust, excess income is placed into the trust. Essentially, the income in the trust goes to pay for long-term care, but is not counted as income for income cap purposes. This is a legal fiction that makes no logical sense, but it works.
2.2.4.2. Types
All types of income are counted including wages, social security, pensions and annuities, alimony, interest and dividends.[7]
2.2.4.3. Name on Instrument Rule
The name on instrument rule applies in determining to whom income belongs. If there is a joint “and” account, income is deemed to belong one-half to each. If it is a joint “or” account, Medicaid takes the position that the entire account belongs to the applicant.[8]
2.3. Minimum Monthly Maintenance Needs Allowance
Medicaid Regulations provide for a Minimum Monthly Maintenance Needs Allowance which is composed of $1,991.25 per month adjusted annually on July 1 of each calendar year, plus the community spouse’s expenses for rent, mortgage, taxes, insurance and certain utilities in excess of $597.38 per month. These figures are for the period July 1, 2015 through June 30, 2016.[9] The maximum MMMNA is currently $2,980.50.[10]
2.4 Resources
2.4.1. Cap
Resources cannot exceed $2,000.[11]
2.4.2. Excluded Resources
2.4.2.1. Home
The primary residence and lot are excluded if occupied by the institutionalized person or the community spouse. Absence of more than six months creates a presumption that the home no longer serves as the principal residence.[12] However, states may establish a cap on the equity of the home. The minimum cap is $552,000 and the maximum cap is $828,000.[13]
2.4.2.2. Automobile
One automobile is exempt.[14]
2.4.2.3. Personal Effects and Household Goods[15]
2.4.2.4. Wedding Ring and Engagement Ring[16]
2.4.2.5. Medical Equipment
Needed by an institutionalized person or a member of his household.[17]
2.4.2.6. Burial Fund
A prepaid funeral is permitted provided the funeral director places the payment in an irrevocable trust for this purpose or, provided that a life insurance policy is irrevocably assigned to the funeral director.[18]
2.4.2.7. Inaccessible Resources
Resources which cannot be liquidated are considered inaccessible resources.[19]
2.4.2.8. Term Life Insurance[20]
Term life insurance is not countable since it has no cash value.
2.4.2.9. Whole Life Insurance with a maximum face of $1,500[21]
2.5. Pooling
Resources owned individually by the institutionalized spouse and the community spouse or owned jointly by the institutionalized spouse and the community spouse are pooled together to determine Medicaid eligibility. However, this rule does not apply to a spouse who entered a nursing home prior to September 30, 1989.[22] Transfers between such spouses, are permitted without resulting in any period of ineligibility.
2.6. Transfer of Resources
2.6.1. Look-Back Rule
There is a 5-year look-back for transfers of assets.[23] This means that the disposal of resources, for less than fair market value, in the 5-year period prior to the month of application must be reported at the time of the Medicaid application. Transfers made beyond the look-back period are not penalized. Transfers within the look-back period are penalized.
2.6.2. Penalty
2.6.2.1. Transfer Penalty
To calculate the penalty, divide the amount of the transfer by the average cost of nursing home care in New Jersey, $10,116.28, or a daily rate of $332.59, in 2015.[24] Under the Deficit Reduction Act, the penalty is calculated in partial months.[25] The penalty is the period for which the institutionalized spouse would be ineligible for Medicaid. Under federal law, the penalty is unlimited.[26]
2.6.2.2. Beginning Date
The penalty begins on the later of the date of the transfer for less than fair market value, or the date on which the individual is eligible for medical assistance under the State Plan and would otherwise be receiving institutional-level care based on an approved application for such care but for the application of the penalty period, whichever is later and which does not occur during any other period of ineligibility.[27] Therefore, the penalty begins when a person is actually receiving care, has reduced his or her resources to $2,000, and has no other penalty outstanding.
2.6.2.3. Transfers by Community Spouse
Transfers by the community spouse are also subject to the same penalty as transfers by the institutionalized individual.
2.6.3. Exemptions from Transfer Penalty
Exemptions from the transfer penalties period are:[28]
(1) Transfer to the community spouse or for the sole benefit of the community spouse.
(2) Transfers to a blind or disabled child or for the sole benefit of a blind or disabled child.
(3) Transfer of a principal residence to:
(a) Community spouse.
(b) Child under 21, blind or disabled.
- Child who is residing in the house for at least two years, and who had provided care for the parent, allowing the parent to stay at home.
- Sibling who also has an ownership interest in the house, and who is residing in the house for at least one year.
2.7. Community Spouse Resource Allowance
This guarantees the community spouse a minimum amount of resources without affecting the institutionalized spouse’s Medicaid eligibility. For 2016, this is the greater of $23,844 or one-half of the couple’s non-exempt resources not to exceed $119,220.[29] These figures are adjusted on January 1 of each calendar year.
2.8. Snapshot
The determination of a couple’s resources is made at the time the institutionalized person begins to receive a “nursing home level of care” or at the time of the Medicaid application, whichever first occurs. A nursing home level of care could be care at home or in an assisted living facility or in a nursing home. This determination is used to establish the Community Spouse Resource Allowance.[30]
2.9. Taxation
In doing Medicaid planning, income tax, gift tax and estate tax consequences need to be considered, including medical deductions, personal dependent exemptions, carry-over basis, and step-up in basis.
2.9.1. Income Tax
2.9.1.1. Medical Deduction
The IRS permits an income tax deduction for medical expenses. Medical expenses include qualified long-term care services.[31] Qualified long-term care services are defined in the tax code[32] as “necessary diagnostic, preventive, therapeutic, curing, treating, mitigating and rehabilitative services, and maintenance and personal care services, which: (a) are required by a chronically-ill individual, and (b) are provided pursuant to a plan of care prescribed by licensed health care practitioner.” A chronically-ill individual is a person certified by a licensed health care provider as being unable to perform two activities of daily living for a period of at least 90 days. The activities of daily living are defined to mean “eating, toileting, transferring, bathing, dressing and continence.” The Conference Report notes “It is intended that an individual who is physically able, but has a cognitive impairment such as Alzheimer’s disease, or other form of irreversible loss of mental capacity, be treated similarly to a person who is unable to perform at least two activities of daily living.”
A taxpayer can claim an itemized deduction for unreimbursed medical expenses to the extent such expenses exceed 10% of adjusted gross income. Qualified long-term care services, insurance premiums and other eligible medical expenses may be aggregated.
Except for insulin, expenditures for medicine and drugs are deductible only if prescribed by a physician.
Capital expenditures are deductible if they are medically necessary and represent an unrecoverable sunk cost. To the extent the purchase increases the value of an asset, the expenditure is non-deductible regardless of the degree of medical need. The IRS has published a list of home modifications that are deemed not to add to a home’s value.[33]
Personal care services are tax deductible, if provided pursuant to a plan of care prescribed by a licensed health care practitioner (i.e., physician, registered nurse, geriatric care manager). Expense must be primarily related to needed assistance with any of the disabilities for which the individual qualified as chronically ill or cognitively impaired. Examples include expenses related to a patient’s dressing, grooming and bathing, if an individual is unable to perform those functions without assistance. There is no deduction for what might be termed “maid” services. These include cooking and general cleaning.
Payments for qualified long-term care services provided by an individual do not qualify as paid-for medical care if the service is provided by the spouse of the individual or by a relative, unless the service provider is a licensed professional with respect to the service.
2.9.1.2. Personal Dependent
If a person pays for more than 50% of the support of a relative, and the relative in calendar year 2016 has less than $4,050 of gross income for the year and has not filed a joint return with his or her spouse, then the person paying the support may claim the relative as a dependent on the person’s federal income tax return.[34] For purposes of calculating the 50% requirement, tax-exempt interest income, disability income and Social Security income, of the relative is counted. However, for purposes of calculating the $4,050 of gross income, tax-exempt interest income, disability income and Social Security income are not counted. If a person claims a relative as a personal exemption, the relative must not file a joint return.[35]
The personal exemption amount for taxable years beginning in 2016 is $4,050.[36]
2.9.1.3. Medical Deduction – Relative
Under the Federal tax code[37] a person can claim a medical deduction for medical expenses paid on behalf of a relative, if the person provided over half of the relative’s total support for the calendar year. The person can deduct the medical expense of the relative, even if the person cannot claim the personal dependent exemption because the relative received $4,050 or more of gross income in calendar year 2016.[38]
A relative is defined[39] as “a child or descendant of a child; stepchild; brother, sister, by whole or half-blood; stepbrother, stepsister; father, mother or ancestor of either (grandparent, great-grandparent, etc.); stepfather, stepmother; nephew, niece; brother or sister of father or mother (uncle, aunt); brother-, sister-, father-, mother-, son-, or daughter-in-law.”
The taxpayer claiming the exemption must, in combination with other taxpayers (i.e., children), provide more than half of the support of the dependent individual for the calendar year. The taxpayer claiming the dependent must have individually provided more than 10% of the individual’s support. The taxpayer must sign a Multiple Support Agreement Form 2120 if:
(1) The taxpayer provided less than half of the dependent’s support for the
calendar year; but
(2) The group provided more than half of the support; and
(3) No one person furnished more than half of that support; and
(4) The taxpayer contributed more than 10% of the support; and
(5) Each person in the group contributed more than 10% signs a
written declaration (Form 2120 can be used) that he/she won’t
claim that individual as a dependent for any tax year beginning
in the calendar year.[40]
All of the declarations must be attached to the return of the taxpayer claiming the dependency deduction.[41]
2.9.1.4. Dependent Care Credit
This is available to a child on behalf of a dependent parent although the parent has more than $4,050 of gross income in calendar year 2016.[42] However, the parent must be physically or mentally incapable of providing self-care (i.e., cannot provide for his or her own hygiene or nutritional needs, or needs the full-time attention of another person for the parent’s safety or the safety of another). The purpose of the credit is to reimburse for care expenses related to the taxpayer leaving home to take employment. Taxpayers are usually better off taking the care expenses as a medical expense deduction.
2.9.1.5. Carryover Basis
In determining which assets to transfer and which assets to retain, consideration must be given to the fact that the donee of a gift receives a “carryover basis.”[43] This means that the cost basis of the donee is the same as the cost basis of the donor. Therefore, when the transferred assets are sold, the donee must pay capital gains tax. The best strategy is, usually, to transfer unappreciated assets to the donee, and reserve appreciated assets for the donor. That way, any gain on the sale of the appreciated assets can be offset by deducting the cost of the nursing home from income tax.
2.9.1.6. Step Up in Basis
Assets forming a part of the estate of a decedent are included in that person’s estate for federal estate tax purposes. The beneficiary of the estate receives a “step up” in basis with respect to those assets so that the beneficiary’s new basis is the fair market value of the assets as of the date of the death of the decedent.[44] The strategy, therefore, is to not sell the home during your lifetime so that your children receive a step up in basis with respect to that property on your death.
2.9.1.7. Retirement Plan
If either spouse has a retirement plan, such as an IRA or savings plan, the withdrawal of funds from that account is a taxable event. If some period of private payment to the nursing home is required, it makes sense to use the money in the retirement plan for this purpose. The medical deduction for the qualified long-term services can be used to offset the taxable income resulting from the withdrawal from the retirement plan.
2.9.1.8. Deferred Annuity
If either spouse has a deferred annuity, the withdrawal of funds from the annuity is a partially taxable event. That portion of the payment representing the initial purchase price of the annuity is a return of principal and is non-taxable, but the accrued income is taxable. If some period of private payment in the nursing home is required, it makes sense to use the money in the annuity for this purpose. The medical deduction for the qualified long-term services can be used to offset the taxable income resulting from the withdrawal from the retirement plan.
2.9.1.9. Interest on Series E, Series EE and Series I Bonds
At the time Series E, EE or I bonds are redeemed, income tax is due on the accumulated interest.[45] The same is true if the bonds are transferred to another person. Generally, it would be better not to cash in the bonds until such time as the proceeds of sale of the bonds are needed to pay for the nursing home. This is because the medical deduction for the nursing home expense will offset the taxable income from the redemption of the bonds.
2.9.1.10. Domestic Help
Withholding of Social Security and Medicare taxes is required of all employees receiving cash wages of $1,900 or more in calendar year 2016.[46] If the employee receives total cash wages of $1,000 or more in any calendar quarter in 2016, federal unemployment taxes must also be withheld. The first $7,000 of cash wages is subject to federal unemployment (FUTA) in 2016.[47] After an employee reaches $7,000 during the year, the FUTA tax is no longer required. The employer is not required to withhold federal income taxes from the wages paid to household employees unless the employee so requests and the employer agrees. The employee must give the employer a completed W-4, an Employee’s Withholding Allowance Certificate. If there is an agreement for withholding for income taxes, either party may end it by written notice to the other.[48]
If household help is obtained through an agency, the agency is generally responsible for paying the tax, but this must be verified with the agency.
2.9.1.11. Gain on Sale of Home
2.9.1.11.1. General
There is an exclusion[49] from gross income for the sale of a principal residence, if the property was owned and used by the taxpayer as the taxpayer’s principal residence for two of the five years preceding the date of the sale. The amount of the gain excluded is $250,000 for a taxpayer filing individually and $500,000 for taxpayers filing jointly. In the case of married couples, the ownership requirement can be met by either spouse, but both spouses must meet the use requirement, and neither spouse has claimed the exclusion during the two-year period ending on the date of the sale. This provision is applicable to sales on or after May 7, 1997.
2.9.1.11.2. Joint Returns
In the case of joint returns, the exclusion applies if either spouse meets the ownership and use requirements.
2.9.1.11.3. Divorce
If a taxpayer obtains property from a spouse or a former spouse incident to a divorce, the period that the taxpayer owns the property will include the period that the spouse or former spouse owned the property. A taxpayer is treated as using the property as the taxpayer’s principal residence for any period that the taxpayer has an ownership interest in the property and the taxpayers’ spouse or former spouse is granted use of the property under a divorce or separation instrument provided that the spouse or former spouse takes the property as his or her principal residence.
2.9.1.11.4. Determination of Use During Periods of Out-of-Residence Care
A taxpayer who owns property during the five-year period, but who resides in any facility, including a nursing home licensed by a state, counts the time residing in the nursing home as use of the property.
2.9.1.11.5. Residences Acquired in Rollovers Under Section 1034
If a residence is acquired under a Section 1034 rollover, the time periods during which the taxpayer owned and used the former property are counted.
2.9.1.11.6. Repeal of Non-Recognition of Gain on Rollover of Principal Residence
Section 1034 (relating to rollover of gain on sale of principal residence) is repealed.
2.9.2. Gift Tax
If transfers are made in excess of $14,000 per person per year, then a Gift Tax Return will have to be filed by April 15th of the calendar year following the date of the gift. There is an annual exclusion for gifts of $14,000 per person per year or less.[50] If a spouse consents, the annual exclusion gift may be increased to $28,000 per person per year. In addition, there is a gift tax exemption of $5,450,000 for an individual and $10,900,000 for a married couple,[51] so no tax will be due for gifts which do not exceed the amount of this gift tax exemption. There is no tax due from the recipient of the gift. The $14,000 annual exclusion gift will be indexed for inflation in the future.
New Jersey does not have a gift tax. However, New Jersey does have an inheritance tax for assets which are left to persons other than a spouse or lineal ascendants and descendants. If a transfer is made to someone other than a spouse or lineal ascendants and descendants within three years of the date of death, this constitutes a transfer which falls within the scope of the New Jersey Inheritance Tax. In that situation an Inheritance Tax Return must be filed and the appropriate tax paid.[52]
2.9.3. Estate Tax
For persons dying in calendar year 2016, there is a federal estate tax exemption of $5,450,000 for 2016. This is indexed to inflation.[53]
2.9.4. New Jersey Estate Tax
There is a New Jersey estate tax exemption equivalent of $675,000, which means that New Jersey estate tax is not due for estates of $675,000 or less.[54]
2.10. Use of Trusts and General Powers of Attorney in Planning for Medicaid Eligibility
2.10.1 Advantages of Using a Trust over Outright Gifts to Other Individuals
2.10.1.1. Control
The trust allows the grantor to direct, in advance, how the transfer of property is to be managed administered and distributed thereby allowing some control.
2.10.1.2. Risk Avoidance
By transferring assets to trusts as opposed to outright to children, the risk of a child’s creditors attaching the transferred assets or having the assets become involved in a divorce are eliminated. The child would not have declare the transferred assets on a financial aid application, if they are held by a trust.
2.10.1.3. Tax Benefits
Qualification of the trust as a grantor trust allows the grantor to be taxed on the income earned by the trust at the grantor’s marginal income tax rate even if the income is not distributed to the Grantor.
2.10.1.4. Step-up in Basis
If the trust assets are included in the grantor’s estate, the trust principal will be included in the grantor’s estate at death and will receive a step-up in basis at that time.[55]
2.10.1.5. Exclusion from Capital Gain on Sale of Principal Residence
The $250,000 – $500,000 exclusion from capital gain on the sale of a principal residence can be preserved through a properly-structured trust.
2.10.2. Trust Buster Statute
The statute provides “Any provision in a contract of insurance, will, trust agreement or other instrument which reduces or excludes coverage or payment for goods and services to an individual because of that individual’s eligibility for or receipt of Medicaid benefits shall be null and void, and no payment shall be made under this act as a result of such provision.” This statute has never been tested in court. This statute appears only to apply to instruments which provide for mandatory distributions which are then cut back when the individual applies for Medicaid. Example: “Upon the beneficiary applying for Medicaid, all income payments to him shall terminate.”[56]
2.11. Medicaid Transfers by Power of Attorney
It is necessary to explore the capacity of the client to make transfers. If the client lacks the necessary mental capacity, the transfers may, nevertheless, be accomplished through a Power of Attorney, if the document so authorizes. Under New Jersey law gifts are not permitted by an attorney-in-fact except to the extent that the Power of Attorney expressly and specifically so authorizes.[57]
The next problem with a Power of Attorney is whether the agent has authority to make gifts to himself. The agent is a fiduciary. If the Principal wants the agent to be able to self-deal when making transfers for Medicaid purposes, the Power of Attorney should explicitly authorize such gifts. However, authorization of an agent to make gifts to himself under a Power of Attorney, might be considered a general power of appointment.[58] The power of appointment would then cause the assets of the principal to be includable in the agent’s gross estate for federal estate tax purposes.[59] One solution would be to have the Power of Attorney name a special agent with authority to make transfers to the regular agent. An alternative might be through obtaining court approval. A third way might be to put conditions in the Power of Attorney as to when the agent might have the right to self-deal.
2.12. Medicaid Planning by Guardians
Guardians are authorized to make transfers for the purpose of obtaining Medicaid eligibility. In the case of In the Matter of Mildred Keri,[60] the Supreme Court held that a guardian may make transfers for purposes of obtaining Medicaid eligibility for a ward. The Court imposed a five-point test:
- The spend down plan must not interrupt or diminish an
incapacitated person’s care.
- The plan involves transfers to natural objects of the
person’s bounty.
- The plan does not contravene an expressed prior intent
or interest.
- The plan clearly provides for the best interests of the
incapacitated person.
- The plan satisfies the law’s goal to effectuate decisions
an incapacitated person would make if he or she were
able to act.
It is wise to consider making transfers, which are consistent with the estate planning goals of the client. If inconsistent transfers are made, they may result in litigation from beneficiaries of the estate who consider themselves to be treated unfairly.
2.13. Strategies
2.13.1 The Home
- Transfer home to Community Spouse
- Transfer home and retain life estate
- Transfer home and reserve right to use and occupy
- Family reverse mortgage
- Transfer home to grantor trust
- Sale of remainder interest in home
- Purchase life estate
2.13.2 Spend Down
- Pay off debts
- Pay for services
- Prepay real estate taxes
2.13.3 Convert Countable Assets to Non-Countable Assets
- Buy household goods or personal effects
- Make home improvements
- Purchase life estate from children
- Prepaid funeral
- Buy more expensive home
- Purchase Annuity?
2.13.4 Transfer of Assets
- Large transfer of assets
- Care Agreement
- Income Only Trust
- Children’s Trust
- Disability Annuity Trust
- Disability Annuity Special Needs Trust
2.13.5 Divorce
2.13.6 Hardship Waiver
- LONG-TERM CARE INSURANCE
Long-term care insurance can be helpful to clients who are healthy enough and affluent enough to afford it. As Elder Law attorneys, we must all be aware that Medicaid and other public assistance programs may not continue to exist in the future as we know them today. It would be a disservice to our clients to advise them to rely on these programs in the future. Clients who can afford long-term care insurance and who may be insurable, should be urged to consider purchasing the insurance. Premiums for nursing home insurance can be controlled to a certain extent by the client. The features which affect the premium cost, which can be selected by the client, are the maximum daily benefit, the elimination period, the benefit length, the inflation rider and the amount of home care covered. There are two factors that the client cannot control, which greatly affect the premium. These are the client’s age at application and health history. For this reason, clients should purchase long-term care insurance at the earliest possible time. Most experts consider that the best time to purchase long-term care insurance is about age fifty.
Congress provided tax deductions[61] and tax relief for “qualified long-term care insurance contracts.” New Jersey has regulations concerning long-term care insurance contracts.[62]
It is estimated that only 6% to 8% of the elderly have private long-term care insurance.[63] There are four reasons why people do not buy long-term care insurance:
- Lack of Awareness – The industry has not done a good job in marketing this product.
- Denial – 77% of people surveyed by the American Council of Life Insurance believed they would be healthy in retirement.[64]
- Cost – It is estimated that only 10% to 20% of the elderly can afford such insurance.[65]
- Insurability – Many people wait until they have a diagnosis before applying for long-term care insurance. At that point, they are no longer insurable. Agents estimate that approximately 25% of persons applying are rejected for health reasons.
3.1. Nursing Home Insurance Factors
3.1.1. Coverage
Policies need to be carefully analyzed to see if there are exclusions for alcohol and drug abuse related services or mental health related services. New Jersey requires that all policies include coverage for Alzheimer’s and other organic brain disorders.
3.1.2. Premiums
Premiums for long-term care insurance are high. However, the cost of the premiums is relatively low compared to the cost of payment for a nursing home. Each family must make the premium fit within its family budget.[66] The earlier the policy is purchased, the more affordable the premium.
Most long-term care insurance policies are guaranteed renewable. This means that coverage cannot be canceled by an insurance company, nor can premiums be raised on an individual basis, because of increasing age or declining health. Premiums can be raised only on a class basis affecting all policyholders with that insurance company in that class, and then only with the approval of the state insurance department. In practice, premiums are seldom, if ever, raised on this basis.
3.1.3. Daily Coverage
Persons buying long-term care insurance usually purchase a policy which reimburses their long-term care costs up to a selected maximum amount per day. For example, in this area many people purchase $350 per day of coverage. The actual average cost of a nursing home in New Jersey in 2016 averages close to $400 per day for the basic rate. Ancillary charges such as medications and incontinent care are extra. The difference is made up by the individual’s Social Security, pension or other income.
Some policies are written as a pool of money. An individual might purchase $638,750 of coverage. This is the equivalent of $350 per day coverage for five years ($350 x 365 days x 5 years = $638,750).
3.1.4. Gatekeepers
Companies can sell qualified or non-qualified policies. Qualified policies offer certain safe harbor tax benefits. The primary advantage of a tax-qualified policy is that the benefits paid under the policy are clearly not taxable income. The disadvantage of a tax-qualified policy is that the figures for coverage are more difficult to achieve. Many agents sell only tax-qualified policies.
For a long-term care insurance policy to be a qualified contract, it must provide for benefit eligibility to be determined by meeting a chronically-ill individual standard. The term “chronically-ill individual” means an individual who has been certified by a licensed health care practitioner as being unable to perform at least two of the activities of daily living (ADLs) and whose disability is anticipated to last for a period of at least 90 days due to a loss of functional capacity; or, requiring substantial supervision to protect such individual from threats to health and safety due to severe cognitive impairment.[67] There are two triggers under the new law. The ADL Trigger and the Cognitive Impairment Trigger.
3.1.4.1. ADL Trigger
The activities of daily living (ADLs) include eating, toileting, transferring, bathing, dressing and continence. The long-term care insurance policy must take into account at least five of such activities. The inability of the insured person to perform two of the five or two of the six ADLs without substantial assistance triggers eligibility under the policy.[68] The 90-day period is not a waiting period. The 90 days can be prospective and does not affect the elimination period.
3.1.4.2. Cognitive Impairment Trigger
Severe cognitive impairment means a deterioration or loss in intellectual capacity that is measured by clinical evidence and standardized tests which reliably measure impairment in short- or long-term memory; orientation to people, place or time; and deductive or abstract reasoning. The deterioration or loss must place the individual in jeopardy of harming himself or others and, thereby, require substantial supervision by another individual. A person who is physically able but has cognitive impairment such as Alzheimer’s Disease or another form of irreversible loss of mental capacity is treated similarly to an individual who is unable to perform (without substantial assistance) at least two ADLs.
The IRS defines substantial assistance as “hands-on assistance and stand-by assistance.”[69] “Hands-on assistance” means the physical assistance of another person without which the individual would be unable to perform the ADL. “Stand-by assistance” means the presence of another person within arms’ reach of the individual that is necessary to prevent, by physical intervention, injury to the individual while the individual is performing the ADL (such as being ready to catch the individual, if the individual falls while getting into or out of the bathtub or shower as part of bathing, or being ready to remove food from the individual’s throat, if the individual chokes while eating). An individual is chronically-ill only if a licensed health care practitioner has certified that the individual is unable to perform (without substantial assistance from another individual), at least two ADLs for a period anticipated to last at least 90 days due to loss of functional capacity. A licensed health care practitioner is a physician, registered professional nurse, licensed social worker, or other individual who meets requirements that may be prescribed by the IRS.[70]
3.1.5. Inflation Provisions
Nursing home costs in New Jersey increase faster than the general rate of inflation. Some homes increase annually, some more often. A daily benefit of $250 purchased today may be sufficient now, but may be inadequate five years from now when the client enters a nursing home. Therefore, inflation coverage should be considered.
Some policies have inflation riders which offer increases based on the Consumer Price Index (CPI). Insureds are offered the right to purchase additional coverage at their attained age. Premiums increase when high coverage is elected. Other companies offer policies with an inflation rider which increases coverage automatically at 5% per year, either on a simple or a compounded basis. Automatic inflation riders keep premiums level as benefits increase. Nursing home costs increase on a compounded basis, so an inflation rider, which increases on a compounded basis, is best.
3.1.6. Pre-Existing Conditions
New Jersey LTC regulations define a “pre-existing” medical condition as any condition for which the applicant received advice or treatment during the six month period prior to making application. Further, if an applicant is accepted, a company cannot impose a pre-existing medical condition waiting period on the insured person for more than six months from the effective date of coverage. Persons with diagnosed Alzheimer’s or Parkinson’s Diseases will always be denied coverage. However, persons with histories of cancer, heart disease or similar conditions are often able to obtain coverage. The insurance companies generally like to see a period of time during which it is clear that the condition is controlled. In some instances, the coverage is obtained at regular rates. In other instances, the coverage is granted, but the client is rated, which means that the client pays a higher insurance premium or is offered a shorter benefit length or a longer deductible.
3.1.7. Benefit Length
The benefit length is the period of time which the insurance company will pay after the client starts receiving benefits for long-term care. Coverage is available for two years, three years, four years, five years, six years or unlimited. The longer the term of coverage selected, the more expensive the premium. Attorneys often advise clients to obtain three or four years of coverage. This enables the client to do public assistance planning and, under current law, all or most of the lookback period is covered by insurance. Because Medicaid, as we know it today, may not be available in the future, it may be well to advise clients to purchase as long a term of coverage as they are able to afford.
3.1.8. Guaranteed Renewability
It is important that a policy be guaranteed renewable. If a client purchases a policy when healthy, and is later diagnosed as having a condition such as Alzheimer’s, the client needs to have the assurance that his coverage cannot be canceled or his premium individually raised. Federal law now requires that qualified policies be guaranteed renewable.[71]
3.1.9. Home Heath Care
Most companies have comprehensive, “bundled” policies which include home health care. Some companies have home health care riders which can be added to the basic nursing home/assisted living facility coverage. At least one company has a policy which covers only home health care. Clients do not want to spend time in nursing homes. They would much prefer to stay at home. It is important to obtain home health care coverage so that the family can afford to keep the client at home.
3.1.10. Waiver of Premium
Some policies waive the payment of premiums when benefits are being received or have been received for a given period of time, typically 90 days. Premiums normally resume once benefits stop being paid.
3.1.11. Case Management
Some long-term care insurance policies offer a benefit option referred to as “case management.” Under case management a professional oversees the care and the services the insured would receive. The case manager may be an insurance company employee. This is managed care for long-term care insurance, and should be carefully analyzed. Other policies allow the client to choose his own case manager.
3.1.12. Adult Day Care and Respite Care
Most LTC policies provide benefits for adult day care services and respite care. Respite benefits allow for immediate coverage while an informal caregiver (wife, daughter, etc.) gets a break.
3.1.13. Quality of the Insurance Company
The quality of the insurance company is important. After paying premiums for a number of years, the client expects the insurance company to pay the claim when made. Because of the experience of Executive Life, Mutual Benefit Life and other insurance carriers which have experienced financial difficulties, it is wise for the attorney to counsel the client to look at the ratings of the insurance companies. Ratings services include the following:
- Moody’s Investors Service
99 Church Street
New York, New York 10007
Telephone: (212) 553-1658
Fax: (212) 553-4062
Website: www.moodys.com
- Standard and Poor’s
25 Broadway
New York, New York 10004
Telephone: 212-208-1527
Fax: 212-208-8571
- Duff and Phelps
55 East Monroe Street
Suite 3500
Chicago, Illinois 60603
Telephone: 312-368-3157
- A.M. Best
Ambest Road
Oldwick, New Jersey 08858
Telephone: 908-439-2200
Fax: 908-439-3296
- Weiss Ratings
4176 Burns Road
Palm Beach Gardens, Florida 33410
Telephone: 561-627-3300 or 1-800-289-9222
Fax: 561-625-6685
3.2. Policy Features
The features of the policy which determine cost are:
3.2.1. Daily Benefit
The daily benefit is the maximum amount of money which the insurance company will pay to the insured for each day of long-term care services.
3.2.2. Elimination Period
The elimination period is like a deductible. It is the number of days which the client is willing to pay privately before the insurance begins. Insurance is available which will pay from the first day of care. Other options are a twenty-day elimination period up to a 100-day elimination period or even 365-day elimination period. The longer the elimination period, the lower the premium. A 100-day elimination period usually makes sense. It can reduce the premium substantially at older ages, and Medicare and Medi-Gap Insurance may cover the 100 days, if the patient meets the Medicare requirements for a skilled nursing facility. If not, the client self-insures.
3.2.3. Benefit Length
The benefit length is the number of years the insurance company will pay the nursing home. The term begins after the client enters the nursing home.
3.2.4. Inflation Rider
A 5% compounded inflation rider is the most expensive, but affords the best coverage because the increases in nursing home rates are compounded.
3.3. Taxation
3.3.1. Income Tax Deduction
Under HIPAA, qualified long-term care insurance premiums are deductible from federal income tax as a medical expense up to certain limits.[72]
While payment for medical services provided by relatives does not ordinarily qualify for a medical expense deduction under I.R.C. §105(b), reimbursements through insurance to a relative for such care do qualify.[73] For example, if Dad, who has Alzheimer’s, hires his daughter, a licensed practical nurse, to care for him, payments from father to daughter are not tax deductible. However, if the insurance company pays the daughter, the payments are not counted as income to the father.
Eligible long-term care insurance premiums for a qualified long-term care insurance contract up to the following dollar limits for 2016 qualify as tax deductible medical expenses.[74]
Attained Age by Yr. End Annual Limit on Prem. Ded.[75]
40 or less $390
41-50 $730
51-60 $1,460
61-70 $3,900
Over 70 $4,870
Unfortunately, this deduction is largely illusory, because it is subject to the overall 10% floor of adjusted gross income on deduction of medical expenses. Most people who are healthy enough to purchase long-term care insurance do not have enough other medical expenses to deduct so that they can hit the 10% threshold. It is likely that the tax deduction will be attained only if one spouse is ill and the other spouse has the insurance.
3.3.2. Exclusion From Taxation of Benefits Under Qualified Contracts
Amounts received as benefit payments under a qualified long-term care insurance contract are treated as amounts received for personal injury or sickness, and as reimbursement for expenses actually incurred for medical care and are, therefore, excluded from income for tax purposes.[76] On flat indemnity policies, there is a limitation of $340 per day for 2016.[77] Amounts greater than this are tax-free to the extent they cover actual costs. The $340 figure will be increased to reflect inflation. It is not clear whether benefit payments made under non-qualified contracts are excludable from gross income.
- MEDICARE[78]
4.1. Requirements
Medicare will pay for nursing home care provided two requirements are met:
- Hospital. The patient must spend three days in the hospital and must be admitted to a
nursing home within 30 days after discharge from the hospital.
- Skilled Care. The patient must be admitted to the nursing home for skilled care on a daily
basis. Skilled care is defined as services that are so inherently complex that they can only be
provided effectively by skilled individuals or under the supervisor of skilled personnel.[79]
4.2. Coverage
Medicare will pay for up to 100 days. However, there is co-insurance from the 21st to 100th day. For 2016, the co-insurance rate is $161 per day[80], which must be paid by either the patient or a Medi-gap policy. The 100 days of coverage are not guaranteed. This is a maximum, not a minimum. If the patient is receiving rehabilitation and hits a plateau, Medicare will be stopped.
- VETERANS BENEFITS
5.1. Federal
A Veteran with a service-connected disability of 70% or more is entitled to free lifetime nursing coverage regardless of means. Veterans who do not have a service-connected disability are means-tested as to payment. The VA does contract with public and private nursing home facilities, in addition to using VA facilities.[81]
5.2. State
5.2.1. General
New Jersey Veterans Administration operates three Old Soldiers’ Homes for New Jersey Veterans and their families. They are located in Paramus, Edison and Vineland. Veterans, spouses of Veterans, surviving spouses, and certain parents may be eligible.[82]
5.2.2. Fee
The Adjutant General determines an “Established Rate” each year. The individual pays a portion of the cost of care based on their monthly income and ability to pay.[83] The VA monthly nursing home fee is 80% of the resident’s net income, not to exceed the Established Rate. In addition, 12% of the remaining 20% of the resident’s net income (maximum $20 per month) is set aside in a Welfare fund at the institution, and the remaining balance is placed in a personal needs account for the resident. Net income is calculated after the deductions discussed below. Income includes all income except for service-connected disability compensation. If a resident sells his home and a portion or all of the proceeds from the sale are not reinvested in a primary residence, any income earned from the investment of any or all of the proceeds will be counted as income.[84]
Certain deductions are permitted to the community spouse. For example, the community spouse receives a flat $700 exemption for food, transportation, clothing, telephone and home maintenance.[85] In addition, deductions requiring verification are permitted for rent, first mortgage payments, real estate taxes and insurance, heat and electric, water and sewer, life insurance for burial accounts, and other extraordinary expenses.
5.2.3. Guardianship or Advanced Directive
A Guardianship or Advanced Directive is required for admission.
5.2.4. Resources
The resource limit for a single person is $24,000, and for a married couple is $110,000.[86]
5.2.5. Look-Back
The Veterans look-back period is effectively 36 months.[87]
- CONCLUSION
Financing nursing home care in New Jersey is a complex enterprise. The rules change quickly and are not always written. Medicaid case workers often feel they have an obligation to protect the public purse, rather than to assist the applicant by suggesting various strategies. Case workers are sometimes poorly trained and do not know various planning techniques. Planning for Medicaid financing of nursing home care offers an excellent opportunity for elder law attorneys to be of assistance to their clients.
Rev. 1-5-16
[1]N.J.A.C. 10:71-3.2.
[2]N.J.A.C. 10:71-3.4.
[3]N.J.A.C. 10:71-3.9.
[4]N.J.A.C. 10:71-3.10.
[5]N.J.A.C. 10:71-3.12(c).
[6]N.J.A.C. 10:71-3.12(a).
[7]N.J.A.C. 10:71-5.1.
[8]N.J.A.C. 10:71-4.1(d)2.
[9]N.J.A.C. 10:71-5.7(c); 80 Fed. Reg. 3236 (Jan. 22, 2015).
[10]2016 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[11]N.J.A.C. 10:71-4.5(c).
[12]N.J.A.C. 10:71-4.4(b)1i.
[13]42 U.S.C. §1396p(f); 2016 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[14]N.J.A.C. 10:71-4.4.
[15]N.J.A.C. 10:71-4.4(3).
[16]N.J.A.C. 10:71-4.4(b)3ii.
[17]N.J.A.C. 10:71-4.4(b)3iii.
[18]N.J.A.C. 10:71-4.4(9).
[19]N.J.A.C. 10:71-4.4(b)6.
[20]N.J.A.C. 10:71-4.4(b)4.
[21]Id.
[22]N.J.A.C. 10:71-4.6.
[23]42 U.S.C. §1396p(c)(1).
[24]N.J.A.C. 10:71-4.10(m)1; Medicaid Communication No.12-16 (Dec. 10, 2012).
[25]Id.
[26]HCFA Transmittal No. 64 §3258.4.
[27] 42 U.S.C. §1396p(c)(1)(D).
[28]N.J.A.C. 10:71-4.10(d).
[29] 2016 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[30]N.J.A.C. 10:71-4.8(a).
[31]I.R.C. §213.
[32]I.R.C. §7702B
[33]Rev. Rul. 87-106, 1987-2 C.B. 67.
[34]I.R.C. §151; Rev. Proc. 2015-53(3)(.24).
[35]I.R.C. §151; Rev. Proc. 2015-53(3)(.24).
[36]I.R.C. §151; Rev. Proc. 2015-53(3)(.24).
[37]I.R.C. §152(c) and I.R.S. Publication 502.
[38]I.R.C. §151; Rev. Proc. 2015-53(3)(.24).
[39]I.R.C. §152(a), (b)1 and Treas. Reg. §1.151-3(a).
[40]I.R.C. §152(c).
[41]Treas. Reg. §1.152-3(c).
[42]I.R.C. §151; Rev. Proc. 2015-53(3)(.24).
[43]I.R.C. §1015.
[44]I.R.C. §1014(b)(9).
[45]I.R.C. §454(c).
[46]78 Fed. Reg. 66413 (Nov. 5, 2013).
[47] I.R.C. §3306(b)(1).
[48]I.R.S. Publication 926 (Jan. 2008).
[49]I.R.C. §121.
[50]I.R.C. §2503. (b); Rev. Proc. 2015-53(3)(.35)(1).
[51]I.R.C. §2010; Rev. Proc. 2015-53(3)(.35)(1).
[52]N.J.A.C. 18:26-5.7.
[53] I.R.C. §2010; Rev. Proc. 2015-53(3)(.33).
[54]N.J.S.A. 54:38-1.
[55]I.R.C. §1014(b)(9).
[56]N.J.S.A. 30:4D-6F
[57]N.J.S.A. 46:2B-8.13a.
[58]I.R.C. §2041(b).
[59]I.R.C. §2041(a)(2).
[60]In the Matter of Mildred Keri, 181 N.J. 50 (2004).
[61]The Health Insurance Portability and Accountability Act of 1996 (HIPAA).
[62]N.J.A.C. 11:4-34.1 to 34.13.
[63]J. M. Wiener, L. H. Illston & R. J. Hanley, Sharing the Burden: Strategies for Public and Private Long-Term Care Insurance, 6 (Brookings Institutions, 1994).
[64]Longevity and Retirement Survey Fact Sheet, American Council of Life Insurance. Survey conducted between August 12 and September 10, 1997.
[65]J. M. Wiener, L. H. Illston & R. J. Hanley, Sharing the Burden: Strategies for Public and Private Long-Term Care Insurance, 14 (Brookings Institutions, 1994).
[66]Health Insurance Association of America LTC Market Survey, 1996.
[67]I.R.C. §7702B.
[68]I.R.C. §7702B(c)(2).
[69]I.R.S. Notice 97-31.
[70]I.R.C. §7702B(c)(4).
[71]I.R.C. §7702B(b)1(C).
[72]I.R.C. §213(d)(1)(D).
[73]I.R.C. §213(d)(11).
[74]I.R.C. §213(d)(1)(D).
[75]I.R.C. §213(d)(10); Rev. Proc.2015-53(3)(.25).
[76]I.R.C. §7702B(a)(2).
[77]Rev. Proc.2015-53(3)(.44).
[78]42 U.S.C. 1395 through 1395xx; 42 C.F.R. Pts. 405 through 489.
[79]42 U.S.C. 1395 through 1395xx; 42 C.F.R. Pts. 405 through 489.
[80]2016Medicare Parts A & B Premiums and Deductible Announced, www.cms.gov.
[81]42 C.F.R. 409.31(b)(3), 409.33(b), 409.35.
[82]N.J.A.C. 5A:5.1 et seq.
[83]N.J.A.C. 5A:5-5.2 and 5A:5-5.3.
[84]N.J.A.C. 5A:5-2.1.
[85]N.J.A.C. 5A:5-5.3.
[86]N.J.A.C. 5A:5-2.2(c); Application for Admission (2014).
[87]N.J.A.C. 5A:5-3.1(a)1iv(3).
Again, the insurance leads you bought from benepath.net, which are chockfull of information, whether they are in the Medicare niche or the group insurance niche, are worth looking up on Twitter. The more you get a sense of who your potential client may be, the easier it is to relate to them and find the right kind of insurance policy to suit their needs.
Be creative. Have fun. Engage others on Twitter or other social media platforms and let them get to know who you are. Personally marketing yourself as well as a product is the best way to cultivate customers and get conversions.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Can I use Twitter to promote my insurance agency? first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
Settlement Protection Trusts can be very useful tools in the settlement of a personal injury case. A Settlement Protection Trust is very flexible. However, it cannot be used where an individual is receiving means-tested public benefits. A Settlement Protection Trust is essentially a Support Trust designed to provide for the health, education, maintenance and support of the trust beneficiary.
A budget is prepared and the trustee can often simply write a monthly check to the beneficiary, so that the beneficiary can pay all of his or her monthly bills. In other cases, the beneficiary will simply obtain a credit card and send the credit card bills to the trustee for payment, so long as the expenditures are within the agreed-upon budget. The budget should be designed so that the money will last as long as the plaintiff lives, if that is possible.
When to Use a Settlement Protection Trust
Minor or Incapacitated Person—Plaintiff Not Receiving Means-Tested Public Benefits
In these situations, a Settlement Protection Trust is ideal. If there is a minor or incapacitated person, the monies can be deposited into the Settlement Protection Trust rather than the probate court.
In cases involving a minor or incapacitated person, the establishment of the Settlement Protection Trust must be approved by the court.
Competent Adult Not Receiving Means-Tested Public Benefits
Where a competent adult is not receiving public benefits, both New Jersey and Pennsylvania allow distributions to be made from income and principal without court approval. The beneficiary enjoys the advantages of the Settlement Protection Trust, and the trust serves to protect the settlement from being squandered by the injured plaintiff or being coveted by family members and friends.
Large Settlement—Client Receiving Means-Tested Public Benefits
In many large settlements, the client may be receiving SSI and Medicaid. In some cases, the Medicaid benefit may be modest and, therefore, unnecessary. In other cases, the Medicaid benefit may be significant, but can be replaced by insurance under the Affordable Care Act or a combination of Medicare and private insurance. In these cases, it is often beneficial to consider giving up the public benefits in exchange for greater flexibility in administration and avoiding the Medicaid payback.
The post USING SETTLEMENT PROTECTION TRUSTS IN PERSONAL INJURY CASES first appeared on SEONewsWire.net.]]>
“If we get some of your bills, do we have permission to pay your medical providers directly?”
That’s a question that I’ve started seeing when GEICO takes recorded statements of some of my clients (and I can only assume that other insurance companies will follow behind). It seems innocuous. The client says, “yes.” Of course, that would be great.
It’s terrible.
Agreeing to this simple request can really hurt your accident claim. Why?
Medical expenses are funny. For most medical providers, there are at least two numbers for medical bills. First, there is the “rack rate” — the full price rate that the medical providers try to charge those without insurance. Second, there is the “insurance rate” — the contractual rate that the medical provider and health insurance companies agree is a proper charge for a particular service. (And in reality, these insurance rates can be different for every different health insurance company, Medicare, Medicaid, and so on.)
Which rate is charged, has an impact on your case.
By offering to pay the bill directly, GEICO and other carriers are trying to get permission to go to your medical providers and try to cut your case out from under you. They’ve paid something they’re going to have to pay anyway, often at a lower rate than you would be able to recover from them, and in the process, they’re decreasing the value of your claim while decreasing their risk. It’s all good to them.
It’s also taking money out of your pocket. If hospital A has a $10,000 bill but is willing to accept $7,500 (and I’m making these numbers up), then if GEICO pays the hospital directly, it saves itself $2,500. However, if the lawsuit goes forward and GEICO has to pay you, the client, the $10,000 and then you pay the hospital the $7,500, then that $2,500 savings goes to you and not the hospital.
So agreeing to this seemingly innocent request is costing you money!
There are a number of ways that an insurance company can use a recorded statement to its advantage. While this is a relatively new tactic, it’s not the only tactic. We always tell our clients that they shouldn’t agree to a recorded statement without having a lawyer present to help protect the clients’ rights.
If you or a loved one has been in a car wreck and have been contacted about a recorded statement, please call us at (512)476-4944 and let us help you before that statement occurs.
The post Insurance Recorded Statement: Beware This Seemingly Innocent Question first appeared on SEONewsWire.net.]]>
Granted, some seniors may not have access to a computer, but a vast majority of today’s elders are fairly proficient with technology. Why not take advantage of that and save yourself some money? Did you know that it’s almost four times less expensive to use internet leads than trying for direct mail leads? Think about how that has the potential to directly affect your bottom line.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Who needs Medicare supplement leads? first appeared on SEONewsWire.net.]]>Again, the insurance leads you bought from benepath.net, which are chockfull of information, whether they are in the Medicare niche or the group insurance niche, are worth looking up on Twitter. The more you get a sense of who your potential client may be, the easier it is to relate to them and find the right kind of insurance policy to suit their needs.
Be creative. Have fun. Engage others on Twitter or other social media platforms and let them get to know who you are. Personally marketing yourself as well as a product is the best way to cultivate customers and get conversions.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Can I use Twitter to promote my insurance agency? first appeared on SEONewsWire.net.]]> 50 Years: What is the Future of Medicare and Medicaid?
50 Years: What is the Future of Medicare and Medicaid?
Fifty years ago, Medicare and Medicaid became the latest and greatest entitlement signed into law. Lyndon B. Johnson did the honors July 30, 1965, with past Democrat president Harry S Truman sitting next to him.
The new law was part of Johnson’s “Great Society” plan, which was a continuation of Franklin Roosevelt’s “New Deal.” It was meant to be another safety net for seniors and other Americans who would need medical care later in life.
It is a significant milestone to have a government program remain operational 50 years later. But with such longevity, the question is then begged, as times have changed:
What will become of this program over the next 50 years?
That discussion has been a hot topic among conservatives and Republicans in regards to saving not only Medicare and Medicaid, but also to Social Security. While those programs were signed into law by Democrat presidents, Republicans have seemed to be the ones fighting to see that the government “upholds its promises to the nation’s seniors.”
With all the talk over the last several years, backed up by various studies and analyses about the programs, there have been suggestions that Medicare and Medicaid may be completely broke as early as 2025 if nothing is done to reform the structure of the system. But there are others who say that sustainability has already been addressed with the Affordable Care Act – though it reportedly took $700 billion from Medicare to pay for the bill.
In some ways, it is serendipitous that these programs have managed to be around for 50 years in the first place. But can the government continue to fulfill promises moving forward as the population ages and there are fewer workers paying into the system but more former workers taking out of the system?
What should be done, if anything has been a source of much debate? And the New York Times, in “celebrating” 50 years of Medicare, opened up its debate and opinion pages to several perspectives about Medicare and its future. While it seems there is general agreement that Medicare will look different in the next 50 years than it was in the last 50 years, there is strong debate as to how the program will change. From discussions about structural reform or developing a single-payer healthcare system (“Medicaid for all,” as it has been deemed), to cutting benefits, raising taxes and having benefits means-tested – there are plenty of options and plenty of areas of discussion and disagreement.
Whichever way you come down, there is one thing that is certain – you can’t be certain about it, so you need to be prepared for alternatives. Before you are near the age of being qualified for Medicare or Medicaid, it would be a good idea to include this topic in your discussion about estate planning with a local certified elder law attorney. He or she can sit down with you and discuss not only your general estate plan to get all your affairs in order, but can also help you understand Medicaid, its uncertain figure and how you can create some certainty for yourself and your family.
When you don’t know how much longer you’ll live, you can’t count on something unreliable. You need a rock to lean on, and your estate plan can be that rock – whether it includes Medicare or not.
The post The Future of Medicare and Medicaid 50 Years from Now appeared first on The Elder Care Firm.
The post The Future of Medicare and Medicaid 50 Years from Now first appeared on SEONewsWire.net.]]> 50 Years: What is the Future of Medicare and Medicaid?
50 Years: What is the Future of Medicare and Medicaid?
Fifty years ago, Medicare and Medicaid became the latest and greatest entitlement signed into law. Lyndon B. Johnson did the honors July 30, 1965, with past Democrat president Harry S Truman sitting next to him.
The new law was part of Johnson’s “Great Society” plan, which was a continuation of Franklin Roosevelt’s “New Deal.” It was meant to be another safety net for seniors and other Americans who would need medical care later in life.
It is a significant milestone to have a government program remain operational 50 years later. But with such longevity, the question is then begged, as times have changed:
What will become of this program over the next 50 years?
That discussion has been a hot topic among conservatives and Republicans in regards to saving not only Medicare and Medicaid, but also to Social Security. While those programs were signed into law by Democrat presidents, Republicans have seemed to be the ones fighting to see that the government “upholds its promises to the nation’s seniors.”
With all the talk over the last several years, backed up by various studies and analyses about the programs, there have been suggestions that Medicare and Medicaid may be completely broke as early as 2025 if nothing is done to reform the structure of the system. But there are others who say that sustainability has already been addressed with the Affordable Care Act – though it reportedly took $700 billion from Medicare to pay for the bill.
In some ways, it is serendipitous that these programs have managed to be around for 50 years in the first place. But can the government continue to fulfill promises moving forward as the population ages and there are fewer workers paying into the system but more former workers taking out of the system?
What should be done, if anything has been a source of much debate? And the New York Times, in “celebrating” 50 years of Medicare, opened up its debate and opinion pages to several perspectives about Medicare and its future. While it seems there is general agreement that Medicare will look different in the next 50 years than it was in the last 50 years, there is strong debate as to how the program will change. From discussions about structural reform or developing a single-payer healthcare system (“Medicaid for all,” as it has been deemed), to cutting benefits, raising taxes and having benefits means-tested – there are plenty of options and plenty of areas of discussion and disagreement.
Whichever way you come down, there is one thing that is certain – you can’t be certain about it, so you need to be prepared for alternatives. Before you are near the age of being qualified for Medicare or Medicaid, it would be a good idea to include this topic in your discussion about estate planning with a local certified elder law attorney. He or she can sit down with you and discuss not only your general estate plan to get all your affairs in order, but can also help you understand Medicaid, its uncertain figure and how you can create some certainty for yourself and your family.
When you don’t know how much longer you’ll live, you can’t count on something unreliable. You need a rock to lean on, and your estate plan can be that rock – whether it includes Medicare or not.
The post The Future of Medicare and Medicaid 50 Years from Now appeared first on The Elder Care Firm.
The post The Future of Medicare and Medicaid 50 Years from Now first appeared on SEONewsWire.net.]]>The difficulty with dementia is not just the emotional cost of watching the person you have known all your life become someone different, but also the financial cost. Just because a person’s brain function weakens doesn’t mean a person’s overall health weakens. There have been plenty of cases where a person will live as many as eight years or more after first being diagnosed with dementia or some related disorder like Alzheimer’s.
Why does that matter? As dementia progresses in a person, he or she will require more and more care that a nursing home can provide. And it could get to a point where that care need is for virtually everything, which Medicare and most long-term care insurance policies can’t cover. When you consider that nursing home care can cost (more commonly) around $90,000 per year, over the course of eight years living with dementia that cost could be $750,000.
Can your nest egg handle that? Fortunately, Medicaid can offset much of the cost, but unfortunately, Medicaid rules are different from state to state – so while the goal may be to keep people in their own homes as much as possible, differing rules may force some people to move to another state in order to better ensure eligibility for Medicaid long-term care benefits. Whether you are able to get Medicaid to pay for long-term care or not, the costs incurred to keep your loved one cared for and relatively comfortable can be appalling.
So whether you are in need of that care in the short-term, or if you are the child who might need to help pay the bill for the care, it is a good idea to meet with a certified elder-law attorney in your area who can help you with your estate plan and give you the best options for your situation in the expectation that dementia may hit your family one way or another. A good estate plan will account for various contingencies in these situations, so you can make sure you have some of your nest egg protected while also being able to meet the financial needs of caring for your elderly loved one when he or she needs it.
The post The Devastating Cost of Dementia appeared first on The Elder Care Firm.
The post The Devastating Cost of Dementia first appeared on SEONewsWire.net.]]>The difficulty with dementia is not just the emotional cost of watching the person you have known all your life become someone different, but also the financial cost. Just because a person’s brain function weakens doesn’t mean a person’s overall health weakens. There have been plenty of cases where a person will live as many as eight years or more after first being diagnosed with dementia or some related disorder like Alzheimer’s.
Why does that matter? As dementia progresses in a person, he or she will require more and more care that a nursing home can provide. And it could get to a point where that care need is for virtually everything, which Medicare and most long-term care insurance policies can’t cover. When you consider that nursing home care can cost (more commonly) around $90,000 per year, over the course of eight years living with dementia that cost could be $750,000.
Can your nest egg handle that? Fortunately, Medicaid can offset much of the cost, but unfortunately, Medicaid rules are different from state to state – so while the goal may be to keep people in their own homes as much as possible, differing rules may force some people to move to another state in order to better ensure eligibility for Medicaid long-term care benefits. Whether you are able to get Medicaid to pay for long-term care or not, the costs incurred to keep your loved one cared for and relatively comfortable can be appalling.
So whether you are in need of that care in the short-term, or if you are the child who might need to help pay the bill for the care, it is a good idea to meet with a certified elder-law attorney in your area who can help you with your estate plan and give you the best options for your situation in the expectation that dementia may hit your family one way or another. A good estate plan will account for various contingencies in these situations, so you can make sure you have some of your nest egg protected while also being able to meet the financial needs of caring for your elderly loved one when he or she needs it.
The post The Devastating Cost of Dementia appeared first on The Elder Care Firm.
The post The Devastating Cost of Dementia first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
Personal Injury attorneys must inquire as to whether their clients are receiving public benefits. Certain benefits are means-tested, so that if the client receives money directly those benefits are reduced or lost completely. This article will outline the common public benefits and indicate whether the receipt of a personal injury settlement will affect those benefits.
Supplemental Security Income (SSI)
Supplement Security Income (SSI) is a means-tested federal program that provides income (a cash assistance grant) to certain aged (65 or over), blind, and persons with disabilities. If an individual has more than $2,000 of assets, he or she will lose SSI. Therefore, the receipt of a personal injury settlement will disqualify the plaintiff from SSI, unless the funds are placed in a Special Needs Trust.
Social Security Disability Income (SSDI)
This program is known as SSDI. It provides an income to disabled workers. It is an insurance program, not a welfare program. Receipt of a personal injury settlement will not affect the plaintiff’s SSDI.
Medicaid
Medicaid is a medical insurance program. There are many ways that individuals qualify for Medicaid. The vast majority of Medicaid recipients receive that benefit, because they are also receiving SSI. If they lose their SSI, they also lose their Medicaid. However, since the Affordable Care Act (ACA), millions of Americans now receive Medicaid regardless of whether or not they are disabled and regardless of whether they are receiving SSI.
For SSI-based Medicaid, there is an asset limit of $2,000. For ACA Medicaid, there is no resource limit. Therefore, receipt of a personal injury settlement by an SSI recipient will cause a loss of Medicaid. However, receipt of a personal injury settlement by a Medicaid recipient who obtained Medicaid through the ACA will not affect eligibility, except that the income from the settlement may push the income of the plaintiff above the income limits for eligibility under the ACA. The solution for an individual receiving SSI-linked Medicaid is a Special Needs Trust.
Medicaid Waiver Programs
Medicaid Waiver Programs are designed to provide Medicaid coverage for long-term care services. These services are typically delivered in the home or assisted living facilities. These services are vital to catastrophically-injured individuals. These programs have an asset maximum of $2,000. Receipt of a personal injury settlement would disqualify the plaintiff from Medicaid Waiver services, unless the funds are placed in a Special Needs Trust.
Medicare
Medicare is a program that pays medical costs of eligible beneficiaries. Unlike Medicaid, which is a welfare program, Medicare is an insurance program. Receipt of a personal injury settlement will not affect Medicare eligibility.
The post PUBLIC BENEFITS CONSIDERATIONS IN PERSONAL INJURY CASES first appeared on SEONewsWire.net.]]>
Mature man reading old book surrounded by heaps of books
SO WHAT IS ELDER LAW?
As you can see on the banner and even in the URL address for this website, we are all about elder law. But perhaps after reading some of this you might be asking, what is elder law anyway?
It sounds like it should be pretty specialized, right?
Well it is, to a point. The specialty is the clientele – those who are older and thus will likely be involved in matters of estate planning, Medicare and Medicaid, Social Security and the like.
No, it is not the legal doctrine of TV lawyer/radio personality Larry Elder.
There are all kinds of attorneys who dabble in various categories of elder law, including those that actually have clientele of varying ages. But there are very few elder law “specialists,” those who at least know a lot about every area of elder law. Elder law can cover the gamut, from estate planning to probate to long-term care to insurance to wills and powers of attorney to nursing home neglect/abuse to Social Security to Medicare and Medicaid.
There are about 13 categories under the umbrella of elder law, and it will be important if you are looking for an elder-law attorney, to understand the right questions to ask to find the attorney who will be the right fit for you. Often it is personality that plays a role, but also it is more about the expertise of that attorney in the particular area of concern that you may have.
What Does an Elder Law Attorney Do?
An elder law attorney can serve as a very important adviser for a senior citizen and/or his or her family in legal and financial matters pertaining to elderly people. Whether it’s planning the estate to setting up long-term care options to powers of attorney, wills and trust – even end-of-life and real-estate issues – an elder law attorney can navigate you and your family through the various issues that will arise at some point.
There are many attorneys who at least dabble in some aspects of elder law, but there are certified elder law attorneys (with the CELA designation) who have a broader and deeper knowledge of the various areas of elder law.
Some people do hire a financial planner and an elder-law attorney for financial and legal matters, respectively, and the two professionals can often work together in consultation. However, if you can only afford to hire one, an elder-law attorney might be the wiser move since many financial issues do have legal guidelines and regulations that an attorney can help interpret – and the attorney would know enough about financial details to be a sound adviser in getting your affairs in order.
If you are in the market for an elder law attorney, try to ask these questions to find the right fit for your particular need:
- How long have you been practicing law (in general)?
- What percentage of time do you dedicate to elder law matters?
- Do you have a specialty within elder law?
- What would I need for our first meeting?
- What is your fee schedule?
No matter what specific need you might have within elder law, a certified elder law attorney can help you with any topic. As many elder law situations involve differing state laws and regulations, it is best to hire an elder law attorney who practices in the state where your elderly family member lives so as to not create confusion and legal troubles later.
Having an elder law attorney, at least on a retainer basis, can be a very sound investment for you and your family for when the inevitable happens, and the transfer of the estate goes on harmoniously and with little to no hassles.
The post What is Elder Law and Elder Law Attorney appeared first on The Elder Care Firm.
The post What is Elder Law and Elder Law Attorney first appeared on SEONewsWire.net.]]>
Mature man reading old book surrounded by heaps of books
SO WHAT IS ELDER LAW?
As you can see on the banner and even in the URL address for this website, we are all about elder law. But perhaps after reading some of this you might be asking, what is elder law anyway?
It sounds like it should be pretty specialized, right?
Well it is, to a point. The specialty is the clientele – those who are older and thus will likely be involved in matters of estate planning, Medicare and Medicaid, Social Security and the like.
No, it is not the legal doctrine of TV lawyer/radio personality Larry Elder.
There are all kinds of attorneys who dabble in various categories of elder law, including those that actually have clientele of varying ages. But there are very few elder law “specialists,” those who at least know a lot about every area of elder law. Elder law can cover the gamut, from estate planning to probate to long-term care to insurance to wills and powers of attorney to nursing home neglect/abuse to Social Security to Medicare and Medicaid.
There are about 13 categories under the umbrella of elder law, and it will be important if you are looking for an elder-law attorney, to understand the right questions to ask to find the attorney who will be the right fit for you. Often it is personality that plays a role, but also it is more about the expertise of that attorney in the particular area of concern that you may have.
What Does an Elder Law Attorney Do?
An elder law attorney can serve as a very important adviser for a senior citizen and/or his or her family in legal and financial matters pertaining to elderly people. Whether it’s planning the estate to setting up long-term care options to powers of attorney, wills and trust – even end-of-life and real-estate issues – an elder law attorney can navigate you and your family through the various issues that will arise at some point.
There are many attorneys who at least dabble in some aspects of elder law, but there are certified elder law attorneys (with the CELA designation) who have a broader and deeper knowledge of the various areas of elder law.
Some people do hire a financial planner and an elder-law attorney for financial and legal matters, respectively, and the two professionals can often work together in consultation. However, if you can only afford to hire one, an elder-law attorney might be the wiser move since many financial issues do have legal guidelines and regulations that an attorney can help interpret – and the attorney would know enough about financial details to be a sound adviser in getting your affairs in order.
If you are in the market for an elder law attorney, try to ask these questions to find the right fit for your particular need:
- How long have you been practicing law (in general)?
- What percentage of time do you dedicate to elder law matters?
- Do you have a specialty within elder law?
- What would I need for our first meeting?
- What is your fee schedule?
No matter what specific need you might have within elder law, a certified elder law attorney can help you with any topic. As many elder law situations involve differing state laws and regulations, it is best to hire an elder law attorney who practices in the state where your elderly family member lives so as to not create confusion and legal troubles later.
Having an elder law attorney, at least on a retainer basis, can be a very sound investment for you and your family for when the inevitable happens, and the transfer of the estate goes on harmoniously and with little to no hassles.
The post What is Elder Law and Elder Law Attorney appeared first on The Elder Care Firm.
The post What is Elder Law and Elder Law Attorney first appeared on SEONewsWire.net.]]>
The post The Medicare "Donut Hole" Explained first appeared on SEONewsWire.net.]]>Seniors and others with Medicare prescription drug coverage (Part D) should be aware of the coverage gap known as the “donut hole,” so that they can plan properly for the cost of their medication.
Most Medicare prescription drug plans have a “donut hole” coverage gap, which means that when you have spent a certain amount on medication, your coverage will be reduced until your costs reach a higher…
Ordering insurance leads to build your agency is easy. Knowing what to order, how many, where and what kind is trickier. Growing an insurance agency takes hard work and dedication. Why mess up your chances at success by ordering leads blindly?
In reality, you do need leads, but where you choose to get them is entirely up to you. Having said that, consider this one important advantage before you try to chase leads on your own or order shared insurance leads.
The leads you chase have not been pre-screened or pre-qualified, so even if they are friends or family, you do not have any idea if they are going to convert. Friends may. Family may. However, there are no guarantees in life.
The same observation is applicable with shared leads from a lead generation company. A potential customer may convert, but chances are low because you are merely one of about seven, or more, agents calling a lead. Wouldn’t it be easier, less time-consuming and more economical to buy exclusive insurance leads that you know will convert, so long as you work them diligently?
If you spend what it takes to make money and carefully select your criteria for ordering quality, relevant leads, you can have the world by the tail. Filter your leads first on paper. To whom do you want to market? What are you marketing? Are you marketing multiple products or one specific product, like Medicare supplement leads? What demographics do you want to target? Where do you want to market your products? How many leads do you want daily, weekly or monthly?
There are other considerations as well. For example, what happens if you get a dud lead? Does the lead generation company you are working with replace that lead? It is important to know, because you are paying for those leads. But more importantly, be aware that not every agent likes the same method of marketing, the same lead generation company or even using the same kinds of leads that another agent does. Some may like aged leads and find they have great success with them. Others prefer real-time leads and make very good money by working them as they come in.
Each to one’s own, but before you know what is your own, do your homework.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Know What You Want Before You Order Insurance Leads from a Lead Generation Company first appeared on SEONewsWire.net.]]>
The post Can I Qualify for Medicare if I have a Disability? first appeared on SEONewsWire.net.]]>Medicare is well-known for providing health insurance for people age 65 and older. However, Medicare can also provide health coverage for younger people with disabilities, so if you have a disability, it is important to know how you may qualify for Medicare. The first step is to apply for disability benefits through the Social Security Administration. To qualify for Social Security disability…
Elder justice was in the spotlight at the conference, which took place nearly a month after World Elder Abuse Awareness Day on June 15. Aging opens adults up to a number of vulnerabilities, such as physical and psychological abuse, neglect and financial exploitation.
According to the White House, a 2010 study revealed that one in 10 older Americans experienced abuse in the previous year. While programs and services such as the National Center for Elder Abuse are available for elderly adults seeking help, policymakers play a key role in raising awareness about elder abuse and working towards prevention.
The conference has taken place each decade since the 1960s to discuss how to improve the quality of life for older Americans. Some of the topics that will be addressed include retirement and financial security, healthy aging, long-term support and elder justice.
This year marks the 50th anniversary of Medicaid, Medicare and the Older Americans Act. Such governmental programs contribute to providing Americans with peace of mind as they age. Older Americans also need access to a well-placed caregiving network, adequate housing and financial security to maintain healthy, independent lifestyles in their old age.
The Obama Administration has participated in listening sessions since July 2014 to learn from aging leaders and older Americans about the key issues that need to be addressed at the conference.
Pioneers of Elder Law – For over 30 years, Gilfix & La Poll Associates LLP has innovated creative legal solutions to help you manage and plan the future of your estate.
To contact an estate planning lawyer visit http://www.gilfix.com/ or call 800.244.9424.
Sylvia Burwell, the Secretary of Health and Human Services, said that the proposed changes set high standards for safety and quality in nursing homes. The proposals were announced as part of the White House Conference on Aging.
Some of the proposals address nursing home abuse. Nurses would be required to be trained in dementia care and preventing elder abuse. There will also be a requirement that nursing homes report staffing levels, which Medicare officials will review to determine whether they are adequate. This stops short of requiring a federal nurse-to-resident ratio, which many advocates had pushed for. Dr. Shari Ling, the deputy chief medical officer for Medicare, said the administration’s approach focused on competency rather than “a numbers game.”
The proposed changes include measures to ensure that families are more involved in the care of their loved ones, as well as rules to promote more individualized care. For instance, residents would be able to choose their own roommates, and requests for meals and snacks at non-traditional times would be accommodated. The proposed rules also address reducing hospital readmissions, minimizing the use of antipsychotic drugs and antibiotics, and strengthening infection control.
If you suspect that a loved one has been abused or neglected at a nursing home, contact Joyce & Reyes for a free consultation to learn more about your rights.
If you need to speak with a Tampa nursing home abuse lawyer, Call Joyce & Reyes at 1.888.771.1529 or visit more of http://www.joyceandreyespa.com/.
The post Administration proposes new rules to help prevent nursing home abuse first appeared on SEONewsWire.net.]]>Original Medicare includes Medicare Part A (hospital expenses) and Part B (other health care such as doctor’s office visits). The monthly premium for most participants is $104.90. Participants also pay “coinsurance” of 20 percent of most medical services.
Medicare Advantage, or Medicare Part C plans, are run by private insurance companies, and must offer comparable coverage to parts A and B. Some Medicare Advantage plans charge the same premium as Original Medicare, but many charge an additional premium. Most also charge coinsurance or a copay (a flat fee for a medical service), and these fees vary from plan to plan.
Original Medicare offers the widest choice of doctors and other health care providers. This may be particularly important to you if you like to travel. Original Medicare also has a lower monthly cost than most Medicare Advantage plans.
Most Medicare Advantage plans cover prescription drugs, which costs extra under Original Medicare. Medicare Advantage plans, by law, have a maximum out-of-pocket expense of $6,700 per year. This can give peace of mind, but most people’s out-of-pocket Medicare spending is far less than this amount. Some plans also offer vision, dental, assisted living and nursing home care, unlike Original Medicare.
The decision to go with Original Medicare or Medicare Advantage can only be made based on the particular terms of the Advantage plan that interests you. Because they are offered by private companies, Advantage plans vary widely in terms of their coverages, premiums, copays and coinsurance fees. Consider carefully the pros and cons of each option and consult with an expert if you need help deciding.
The elder law attorneys at Hook Law Center assist Virginia families with will preparation, trust & estate administration, guardianships and conservatorships, long-term care planning, special needs planning, veterans benefits, and more. To learn more, visit http://www.hooklawcenter.com/ or call 757-399-7506.
The post Choosing between Original Medicare and Medicare Advantage first appeared on SEONewsWire.net.]]>- A health care service, prescription drug, item or supply which you think you are entitled to
receive; - Payment for a health care service, prescription drug, item or supply that you already received;
- A change in the amount you are required to pay for a healthcare service, prescription drug,
item or supply.
You can also file an appeal if Medicare or your plan ceases to offer or pay for your health care service, prescription drug, item or supply. If you are enrolled in a Medicare Medical Savings Account (MSA) Plan, you can file an appeal if you believe that you have satisfied your deductible or you think that a service or item should be applied toward your deductible.
In the event that you decide to file an appeal, request any information that could be helpful to your case from your physician, health care provider or supplier. The appeals process consists of five levels. If you do not agree with the decision reached at any level, you can usually proceed to the next level.
The first step in filing an appeal is to review your Medical Summary Notice (MSN), which lists all of the services and supplies that were billed to Medicare during a time frame of three months. It also reveals the amount paid by Medicare, and the amount you may be required to pay the provider. In addition, the MSN shows whether Medicare has denied your medical claim.
You will receive an MSN by mail every three months. Should you decide to file an appeal, you must do so within 120 days of the day on which you received the MSN in question.
Here are the three ways in which you can file an appeal:
- Complete a “Redetermination Request Form” and mail it to the Medicare contractor.
- On the back of the MSN, there are instructions for you to follow. You are required to mail your
request for redetermination to the firm that manages Medicare claims. - Mail a written request to the firm that manages Medicare claims.
You can also consult an elder law attorney who can help you file an appeal of a claim or reimbursement that was denied.
The elder law attorneys at Hook Law Center assist Virginia families with will preparation, trust & estate administration, guardianships and conservatorships, long-term care planning, special needs planning, veterans benefits, and more. To learn more, visit http://www.hooklawcenter.com/ or call 757-399-7506.
The post How to appeal a Medicare denial first appeared on SEONewsWire.net.]]>Running an insurance business is challenging, fun, frustrating and filled with highs and lows, and yet, those who have chosen to sell insurance products chose to help others be protected for those “what if” moments in life. There is no better job than to help someone select a Medicare supplement that works for him or her and provides the coverage they need. No better feeling than to sell someone final life expense insurance and have them say how thankful they are that their family is now protected.
There are times, though, when trying to juggle all the things you need to do to run an agency gets in the way of working leads. What a dilemma — someone walks in the door that may buy a Medicare supplement policy and you have an inbox full of leads. The customer has been there before, several times, and has not yet made up their mind about what they want. You know you have at least four pre-screened and qualified leads sitting in your computer. Now what?
The best way to manage situations like that is to set firm hours for the various tasks you perform to run your agency. A best practice would be to block off an hour or two each morning to just make phone calls to leads and also have office hours when walk-ins are welcome to drop by to chat.
If you are dealing with a reliable and trustworthy lead generation company, such as Benepath.net, you know without even thinking twice that those leads are ready to convert once you work them. That is what you are paying for when you sign up with Benepath.net. Setting aside time to make those valuable calls means you have a real sense of accomplishment when you are done and likely several sales as well.
If morning hours do not work for you to call leads and set up appointments, then select an hour in the afternoon that works best. If you are calling potential customers about Medicare supplement leads, you may find late afternoon works best. It’s up to you to adjust your timetable to suit those of your clients. Working pre-screened leads means a higher chance of conversions working those leads and if you are doing it during a designated timeframe, you can accomplish the maximum in a window of time prior to dealing with walk-in customers or other necessary appointments.
While there certainly are some best practices when dealing with quality, exclusive leads from Benepath.net, best practices are more a matter of what is best for you and your agency. Finding what that best practice may be is going to take time, trial and error. However, in the long run when you learn to balance the leads with other everyday tasks, success and financial stability is just around the corner.
Benepath is the leading provider of exclusive medicare leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Some Best Practices for Managing Exclusive Medicare Supplement Leads first appeared on SEONewsWire.net.]]>
The post Learn the Facts About Medicare, Medicaid and Long-term Care first appeared on SEONewsWire.net.]]>More than 40 million seniors rely on Medicare for their everyday health insurance needs, and many mistakenly assume that Medicare will also cover long-term care if it is needed. In fact, there are specific limitations to Medicare coverage for long-term care, and such care is often covered instead by Medicaid, which has eligibility requirements. Therefore, it is important to understand how these…
by Thomas D. Begley, Jr., CELA
There are five ways to pay for long-term care:
- Private Pay. The patient or resident simply signs a monthly check.
- Long-Term Care Insurance. Long-term care insurance is the best way to pay for long-term care, but only about 8% of the American population has long-term care insurance. Once someone has a diagnosis of Alzheimer’s, they will no longer be medically eligible for long-term care insurance. Financial Advisors and Attorneys should encourage their clients to purchase long-term care insurance while they are in their 50s. The premiums are less expensive and the client is likely to pass medical underwriting at that time.
- Medicare. Medicare pays very little for Alzheimer’s patients because Medicare only pays for skilled care. Generally, Alzheimer’s patients only require custodial care.
- Veterans Benefits. Certain Veterans and spouses of those Veterans are eligible for Veterans benefits that include federal VA nursing homes, Veterans Aid and Attendance benefits, and state VA benefits. Veterans Aid and Attendance is a monthly check that varies depending on family situation and financial situation as well as the type of service performed by the Veteran.
- Medicaid pays for 40% of long-term care in the United States. Basically, there are four tests for Medicaid eligibility: (1) a medical test, (2) income, (3) transfer of asset test, and (4) resource limits. There is a five-year lookback for Medicaid transfer of assets, so planning should be done long in advance.
“Knowing your products, your sales pitch, what in the most in demand and where to source quality leads and how to work them are all part and parcel of being a top insurance agent. What you don’t get told is how to concisely summarize your agency and its product in less than 30-seconds. It means a laser focus on what is important to tell a potential customer. Can you do it?” asks Benepath.net CEO, Clelland Green, RHU.
Not too many agents can reel off a convincing spiel in 30-seconds, but that does not mean they cannot learn how to. It is a good lesson in marketing and how it works. If an agent can market their agency and what they sell in 30-seconds, they truly understand what it means to market the essentials, and essentials are what customers want.
“They don’t want obscure facts about Medicare supplements, or want to know how much a funeral costs, they want solutions to problems. In other words, just the facts. Getting to the heart of the matter of selling a policy someone actually wants is an art,” adds Green. “This is where knowing your customers wants and needs becomes paramount to making a solid sale.”
What is involved in a 30-second focused pitch, an insurance agency’s digital asset? Quite a lot, and the agent must spend hours scripting, rehearsing, timing and getting feedback on what it sounds like and whether it has the moxie to meet the mark. They need to know their value proposition – what appeals to the customers in the niche they want to market in. It has to highlight a valued product, service or solution, focus on agent expertise and get the message across succinctly but clearly. It is, with practice and patience, doable.
Mini marketing, meaning the 30-second verbal art of telling prospective clients what they need to know about an insurance agency, their products and services has some “must do” components:
- it must include the top three things that make an agency different from the competition
- it must create empathy by identifying a particular group serviced
- it must be short, sweet and to the point because there may not be 60 seconds to make the pitch
- it must transmit enthusiasm for the product and the potential client
- it must aim for a vertical market in one niche, not a broad, all are welcome market
- it must close with a call to action
“The beauty of the 30-second pitch to a client is that you may change it to suit your needs in any industry you choose whether it is group insurance or small business insurance. This helps you refine and define what your agency is about and makes you a driving force to be reckoned with when you are in sales mode,” says Green.
The post Quickly Summarizing an Insurance Agency’s Services and Products – a 30-Second Verbal Art first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., Esquire, CELA
In any recovery involving a personal injury case, the interest of Medicare must be considered.[1] The idea is that because Medicare is a secondary payer, a beneficiary should not be permitted to receive a recovery for future medical care, pocket the money, and then bill Medicare for that future medical care.
Are MSAs Appropriate in TPL Cases?
A Medicare Set-Aside Arrangement (MSA) is never required. In the context of Workers’ Compensation (WC) settlements it is a safe harbor. It should be a safe harbor in the context of Third Party Liability (TPL) settlements as well.
In June 2012, The Centers for Medicare and Medicaid Services (CMS) issued a Notice of Proposed Rulemaking.[2] The rulemaking would outline procedures for MSAs in TPL cases. The American Association for Justice (AAJ) has responded to CMS with respect to this Notice of Proposed Rulemaking.[3] The Notice was submitted to the Office of Management and Budget (OMB) on August 1, 2013. The OMB did not approve the proposed rule and CMS withdrew it on October 8, 2014.[4]
Reasons Supporting the Argument that the Medicare Secondary Payer Act Applies to TPL Cases with Respect to MSAs
There are a number of reasons to believe that MSAs are appropriate in personal injury cases. They are as follows:
- An informal survey of the 10 CMS Regional Offices by members of the Special Needs Alliance confirm that Region has taken the position that even in third party liability (TPL) cases, Medicare’s interests must be considered, and in the absence of further guidance, the Worker’s Compensation (WC) guidelines should be followed.
- The Medicare Secondary Payer Manual now includes language referring to “Liability Set-Aside Arrangement.”
- CMS has issued a memorandum that in TPL cases an MSA is not required “where the beneficiary’s treating physician certifies in writing that treatment for the alleged injury relating to the liability insurance (including self-insurance) ‘settlement’ has been completed as of the date of ‘settlement’ and where future medical items and/or services for that injury will not be required, Medicare considers its interests, with respect to future medicals, for that particular ‘settlement’ satisfied.”[5] The converse would appear to be that if the treating physician will not sign such an opinion letter, the MSA would be required.
- The U.S. Attorney for the Western District of New York has issued a protocol indicating that, under certain circumstances, his office will review MSAs in TPL cases.[6]
- A U.S. District Court[7] has found that a set-aside for future medical expenses in a liability case is appropriate.
Cases Where an MSA is Not Required
There are several situations in which an MSA is unnecessary:
- The facts demonstrate that the claimant is only being compensated for past medicals and not for future medicals. There is no evidence of an attempt to maximize other aspects of the settlement.
- The treating physician concludes in writing that, to a reasonable degree of medical certainty, the individual no longer requires any Medicare-covered treatments related to the claim.
- The client is not receiving Medicare and has no reasonable expectation of receiving Medicare within 30 months. The Medicare Secondary Payer Act does not apply to individuals not covered by Medicare.
Five Alternatives for Personal Injury Attorneys with Respect to MSAs
That leaves practitioners in the same place they were in prior to October 8, 2014. The personal injury attorney, therefore, has five alternatives to consider with respect to an MSA:
- Do nothing to protect Medicare and assume the risk that the rules will be enforced in his case, his client will be denied Medicare coverage for future medicals and possibly bring a malpractice action against the attorney;
- Do nothing but draft releases documenting that the plaintiff has been advised of Medicare’s possible interest and that he knowingly agrees to assume any risk;
- Be prepared to show that Medicare’s interest has been protected by shifting the primary payer – such as a continuing health insurance policy – and assume the risk that the health insurance policy will remain in place and that the person primarily being covered by the policy will not lose his job, die, retire, or become disabled;
- Prepare an allocation report, but do not submit to CMS for approval, and fund the MSA;
- Prepare and submit the MSA to CMS for approval.
The author recommends the fourth alternative to avoid any risk to the client and to the personal injury attorney. If the client does not “consider Medicare’s interest,” Medicare may deny future coverage. If the client files a claim and is denied, he may well bring a malpractice action against the personal injury attorney.
Special Needs Trusts and MSAs
Generally, MSA funds are deposited in a custodial account with a professional trustee or given to the client to self-administer. For cases less than $100,000, giving the funds to the client to self-administer makes sense. CMS has issued a letter of instructions to be delivered to the client who would be administering his or her own custodial account. Even if a client misuses the money, the personal injury attorney should be off the hook with respect to a subsequent malpractice claim.
If the MSA funds are self-administered by the client or administered by a professional custodian and held in a custodian account, they will be considered countable assets that will disqualify the client from asset-tested public benefits such as SSI and Medicaid. The solution to that problem is to deposit the funds in a Special Needs Trust. MSAs are generally administered by custodians such as Medivest. However, money in a custodial account is considered a countable asset for someone receiving asset-tested public benefits. In those situations, a Special Needs Trust (“SNT”) is required and the trust is designed so that the MSA funds are placed in a separate sub-trust within the SNT. Generally, a professional trustee will hire a professional custodian to administer the MSA sub-account. By wrapping the MSA sub-account in the SNT, the assets in that sub-account are no longer countable to the trust beneficiary.
[1] 42 U.S.C. §1395y(b)(2).
[2] 42 C.F.R. Parts 405 and 411; 77 Fed. Reg. 35917-35921 (Jun. 15, 2012).
[3] American Association for Justice (AAJ) in a letter to Suzanne Kalwa of the Centers for Medicare and Medicaid Services (Aug. 14, 2012).
[4] RIN: 0938-AR43 EO 12866 Meetings.
[5] CMS Memorandum, Subject: Medicare Secondary Payer – Liability Insurance (including self-insurance) Settlements, Judgments, Awards, or Other Payments for Future Medical Information, from Acting Director Financial Services Group to Consortium Administrator of Financial Management and Fee for Services Operations (Sept. 29, 2011).
[6] Western District of New York, Medicare Secondary Payer Protocol, Assistant U.S. Attorney Robert G. Trusiak (May 6, 2011).
[7] Big R Towing, Inc. v. Benoit, 211 W.L. 43219 (W.D. La. Jan. 5, 2011).
The post WRAPPING A MEDICARE SET-ASIDE ARRANGEMENT INSIDE A SPECIAL NEEDS TRUST first appeared on SEONewsWire.net.]]>The post CMS finalizes rules for Medicare Shared Savings Program first appeared on SEONewsWire.net.]]>
VA Benefit, but are concerned about what to do with the home.
The typical scenario is that mom was living on her own. She breaks her hip. Goes into the hospital, is discharged to a nursing home for rehab, covered by Medicare. Then from the nursing home the family scrambles to find where she should go, because she can’t go home.
The family decides on an assisted living for mom’s long-term care. At this point, with mom paying $3,000 per month in long-term care costs, the family struggles to find ways to pay for long-term care. They discover the little known VA Benefit that can help pay for long-term care for a surviving spouse. This year that benefit would be $1,149 per month.
However, the VA Benefit has an asset test and the home is an exempt asset so it doesn’t count towards the asset test. But if mom qualifies for the VA Benefit, without any planning, then she has less than $30,000 in her name. As the assets dwindle covering the short fall they look to sell their home.
Wouldn’t Selling the Home Disqualify Mom from her VA Benefits
Wouldn’t selling the home disqualify mom from the VA Benefit? Not if the family takes legal steps to protect the VA Benefit. The family, prior to sale, would consult with a VA elder law attorney who would then create a Veterans Asset Protection Trust and deed the home to the trust. Once the home is deeded to the trust, the home could be sold, and the proceeds of the sale would be available to help pay for mom’s long-term care in her assisted living.
Another Benefit of Placing the Home in a Veterans Asset Protection Trust
Not only would mom be able to maintain her VA Benefit as a surviving spouse of a veteran, she would also be able to protect the proceeds of the home from Medicaid or Nursing Home spend-down. The assets in a Veterans Asset Protection Trust do not count towards the Medicaid asset limit of $2,000, assuming mom makes it long enough without needing Medicaid.
This means that mom, if she needs nursing home level care can qualify for Medicaid to have Medicaid pay her base level of care, while having a pot of resources in her trust to improve her quality of life and pay for additional services.
Next Steps to Protect the Home
If you have a loved one who needs long-term care, could qualify for the VA benefit, and want to sell the home–but are afraid to because of a loss of VA Benefits, then give us a call (888) 390-4360. The Elder Care Firm is the only law firm in Livingston County with a VA Accredited Certified Elder Law Attorney.
The post How to Sell a House and Protect Your VA Benefits appeared first on The Elder Care Firm.
The post How to Sell a House and Protect Your VA Benefits first appeared on SEONewsWire.net.]]>VA Benefit, but are concerned about what to do with the home.
The typical scenario is that mom was living on her own. She breaks her hip. Goes into the hospital, is discharged to a nursing home for rehab, covered by Medicare. Then from the nursing home the family scrambles to find where she should go, because she can’t go home.
The family decides on an assisted living for mom’s long-term care. At this point, with mom paying $3,000 per month in long-term care costs, the family struggles to find ways to pay for long-term care. They discover the little known VA Benefit that can help pay for long-term care for a surviving spouse. This year that benefit would be $1,149 per month.
However, the VA Benefit has an asset test and the home is an exempt asset so it doesn’t count towards the asset test. But if mom qualifies for the VA Benefit, without any planning, then she has less than $30,000 in her name. As the assets dwindle covering the short fall they look to sell their home.
Wouldn’t Selling the Home Disqualify Mom from her VA Benefits
Wouldn’t selling the home disqualify mom from the VA Benefit? Not if the family takes legal steps to protect the VA Benefit. The family, prior to sale, would consult with a VA elder law attorney who would then create a Veterans Asset Protection Trust and deed the home to the trust. Once the home is deeded to the trust, the home could be sold, and the proceeds of the sale would be available to help pay for mom’s long-term care in her assisted living.
Another Benefit of Placing the Home in a Veterans Asset Protection Trust
Not only would mom be able to maintain her VA Benefit as a surviving spouse of a veteran, she would also be able to protect the proceeds of the home from Medicaid or Nursing Home spend-down. The assets in a Veterans Asset Protection Trust do not count towards the Medicaid asset limit of $2,000, assuming mom makes it long enough without needing Medicaid.
This means that mom, if she needs nursing home level care can qualify for Medicaid to have Medicaid pay her base level of care, while having a pot of resources in her trust to improve her quality of life and pay for additional services.
Next Steps to Protect the Home
If you have a loved one who needs long-term care, could qualify for the VA benefit, and want to sell the home–but are afraid to because of a loss of VA Benefits, then give us a call (888) 390-4360. The Elder Care Firm is the only law firm in Livingston County with a VA Accredited Certified Elder Law Attorney.
The post How to Sell a House and Protect Your VA Benefits appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post How to Sell a House and Protect Your VA Benefits first appeared on SEONewsWire.net.]]>
To start, a care plan must be signed off on by a doctor, and the home health agency you’ve selected must be Medicare-credited. In addition, the doctor must certify that you or your loved one is “homebound.”
If you work for a large corporation, chances are the health care part of your retirement package looks a heck-of-a-lot better than a lot of workers employed by a small to-medium size business. Those fortunate enough to have a health package may enjoy a range of bennies, from low medical premiums and extras like dental, hearing aids as well as coverage for eyewear.
To get an idea of just how those employer insurance programs or retiree insurance benefits have withstood the test of uncertain economic times, about 66 percent of retirees were receiving those nice health-care packages back in 1988, compared to only 25% today.
Medical costs will continue its upward trend in retirement.
It’s a depressing fact, but a gloomy forecast looms over the retiree’s Social Security income. In fact, such costs are sure to devour the “majority of retirees Social Security income.”
Are you 66 and planning to retire this year? You might be well served to either work longer or take a part-time job to help pay for health care costs. Surprisingly, notes a new report in the Wall Street Journal, those anticipated medical costs might very well eat up about 67% of a retiree’s benefit in those Golden Years.
If you’re ten years younger and looking to retire ten-years-from-now, count on your medical costs to take away about 90% of your Social Security income in your lifetime.
A simple reason…
Retirees on Social Security grapple with the ever-rising costs of Medicare premiums and skyrocketing medical costs, keeping them on a treadmill of never reaching parity with these costs. But it’s not surprising, given the fact that Social Security’s annual increases are averaging a meager 2%—that’s the current rate of inflation.
But according to Healthview founder, Ron Mastrogiovanni, medical costs are seeing increases from 5% to 7% annually. Unfortunately, those increases did not factor in that Elephant in the Room: long-term care.
Medicare will cover some home health services.
Family caregivers are not only providing for loved ones in time of need, but, ironically, their ‘service’ helps subsidize the Medicare system to the tune of $375 billion annually, according to an Indiana University report,
If you are over 50 years of age and care for a loved one, you are among the 10 million who do. Amazingly, this number has “tripled over the past 15 years,” as noted by a study that included the National Alliance for Caregiving.
“What can Medicare do for my loved one who needs home care?”
But the Medicare program does pick up the following home care costs, including, but not limited to…
— Intermittent skilled nursing care
— Physical therapy, including speech-language pathology services.
— Continued occupational services
Medicare does not pay for…
— 24-hour care at home
— Meals delivered to the home
— On-site homemaker services
— Personal care
What you need for determination…
For starters, a care plan must be signed off on by a doctor, and the home health agency you’ve selected must be Medicare-credited. In addition, the doctor must certify that you or your loved one is “homebound.”
Home health services include other choices.
Depending on where you live, other services can provide for this care, such as medical social services, part-time/intermittent home health aide services. What’s more, the cost of in-home medical supplies and durable medical equipment (walker, wheelchair) and injectable osteoporosis drugs.
Proper estate planning with an experienced elder care attorney, like Christopher J. Berry, can help you better understand the importance of setting aside funds for a long-term care policy; establishing a trust to provide continuity of your assets; creating a power-of-attorney for use if you are incapable of making your own financial and health decisions.
Contact us to learn more.
The post Medicare does pick up some home care costs; best bet is a long-term care policy. appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Medicare does pick up some home care costs; best bet is a long-term care policy. first appeared on SEONewsWire.net.]]> There are six ways to pay for long-term care in Michigan. Fifth out of those six ways to pay for long-term care is the VA Benefit, which in 2015 can pay up to $2,120 per month tax free!
There are six ways to pay for long-term care in Michigan. Fifth out of those six ways to pay for long-term care is the VA Benefit, which in 2015 can pay up to $2,120 per month tax free!
The Six Ways to Pay for Long-term Care
1) Private pay. Pay out of your own assets for long-term care.
2) Kids pay. Typically the children don’t pay financially, but the they pay in term of their time.
3) Medicare. Medicare only pays short term rehab and hospice, not long-term care costs.
4) Long-Term Care Insurance. Long-term care insurance is a tool that can help pay long-term care costs, but it is certainly not a magic wand or the only answer.
5) VA Benefits. We’ll talk more about this more…
6) Medicaid. Medicaid pays for nursing home level care only, with harsh asset qualification penalties.
Michigan VA Benefits For Long-term Care
If a veteran needs long-term care, either home care, assisted living or nursing home care, there is a little known resource called the non-service connected VA Benefit that can help pay that cost of care.
VA Benefits for Home Care in Michigan
Home care in Michigan can easily run over $3,000 per month when you’re buying a couple hours per day a couple times per week. The VA Benefit can easily come in and help off-set some of that cost of care.
Qualification for Michigan VA Benefits
There are five requirements to qualify for the Aid and Attendance Veterans Benefit.
- The Veteran must have served 90 days active duty.
- One of those days must have been during a period of conflict.
- Cannot be dishonorably discharged.
- Long-term Care Costs must exceed Social Security and Pension.
- Asset Test
The benefit is really that straight forward. If you’re able to overcome each of the requirements then you can bring in up to $2,120 per month tax free.
If you would like a free easy action plan to secure your VA Benefits, then contact our office for the VA Benefits Action Plan.
The post Michigan VA Benefits for Long-Term Care Costs appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Michigan VA Benefits for Long-Term Care Costs first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
Nothing is likely to have greater impact on public policy and programs for the elderly than the aging of the Baby Boomers (“Boomers”). Boomers represent 76 million persons in the United States born between 1946 and 1964 – 31% of the total population. Boomers are divided into two waves. The first wave was born between 1946 and 1954 and is currently between 61 and 69 years of age. The second wave was born between 1955 and 1964 and is currently between 51 and 60 years of age. By the year 2030, all surviving members of this generation will be between the ages of 66 and 84 and 90% will be retired by the year 2030.[1] By 2020, close to one-third of the population will be over age 55. Despite the conventional wisdom that Boomers are ready to “work forever” and significantly extend their formal working career, many of the oldest Boomers are already well into the retirement phase. Many more expect to retire upon becoming eligible for full Social Security Retirement benefits.
- Forty-five percent of 65-year old Boomers are now fully retired with another 14% reporting that they are retired but working part-time or seasonally.
- Of those who have not yet retired, 61% plan to retire when they reach 68.5 and are eligible for full Social Security Retirement.
- Forty-five percent of Boomers who retired earlier than planned cited health-related reasons for doing so. Sixteen percent cited loss of a job or job opportunities. Those who retired later than they had planned mentioned needing a salary to pay for day-to-day expenses.
- Sixty-three percent of Boomers have started receiving Social Security benefits prior to reaching full retirement age.
- Seventy percent of retirees report liking retirement “a lot.”
- Twenty-five percent of Boomers received an inheritance from their parents with an average value, before taxes, of $110,000.
As Boomers age, it is useful to study a profile of the average Boomer. MetLife performed such a study.[2] The study showed that the average 62-year old in 2007 was married to the same spouse, who was 60-years old, had 2.4 children over the age of 18 who were not living at home, has two grandchildren also not living in their home, and has no living parents. These individuals tend to have very good health, have some college education, and worked full time. They feel they have done a good job earning income, but a poor job saving for their own future, investing for their children’s future, and ensuring coverage for their long-term care costs. They are politically conservative. They have decided to take Social Security benefits earlier than the normal retirement age. A sizeable portion applies for benefits at age 62 and plan to be fully retired by age 66-years 4 months.
Changes in the global economy have caused a decline in the number of manufacturing jobs in the United States and a move toward service jobs, requiring higher level of skill and education. Fifty-six percent of Boomers will rely on Social Security for over one-half of their income and estimates are that Boomers will save only one-third of the amount required to provide them with a secure retirement at age 65.[3] Further, Boomers have high consumer debt, including education loans, and are borrowing, or will soon need to borrow, to finance their own children’s educations. The National Association of Area Agencies on Aging predicts that, “Baby boomers will have better health in their late 60s and 70s due to better personal care, more healthful work environments, and better health practices throughout their adult lives.”
The retirement of Boomers will put a tremendous stress on the Social Security and Medicare systems. Policymakers, particularly those on the right, will be tempted to reduce benefits to maintain the solvency of both the Social Security and Medicare systems. Such a change would cause serious issues for many Boomers who have retired with no pension, little retirement savings through 401ks, little equity in their homes, and high consumer debt. All of these reasons, and particularly a lack of pensions, makes Social Security even more important to Boomers who are retiring.
The General Accounting Office (GAO) found that an annual drawdown of savings at an annual rate of 4%, coupled with a delay in Social Security, was a good strategy for Boomers to employ for retirement. The longer Social Security is delayed, the higher the monthly payment. Therefore, drawing down on savings first will ultimately lead to a higher monthly check from the Social Security Administration.
There is a dramatic difference between the first wave of Boomers and the second wave. The older wave is better educated and is more likely to be married. The most important source of income for Boomers is earnings from employment, and singled boomers generally earn less than married ones. Also, 71% of first-wave Boomers own their own homes, while only 57% of those in the second wave own homes. As a result, poverty rates in 1990 were one-third higher for those in the second wave of Boomers than for those in the first wave. [4]
According to the National Association of Area Agencies on Aging, large numbers will face economic risk and deprivation, because of a history of low earnings, intermittent employment, poor education, discrimination, and an inability to adjust to changing employer requirements. The most influential variables for a Boomer’s retirement are marital status and level of education.[5]
One of the factors making retirement for many Boomers is the lack of income from pensions. Public sector employees generally receive pensions. Private sector employees generally receive benefits from defined contribution plans, such as 401ks, and 401ks tend to be much less generously funded and pay out much smaller benefits.
[1] P. Berg & A. Collins, Baby Boomers: Issues and Trends Summary Analysis Including Opportunities for the Aging Network, National Association of Area Agencies on Aging.
[2] Highlights of the MetLife Study of Boomers: Ready to Launch, MetLife Mature Market Institute, www.metlife.com (Nov. 2007).
[3] P. Berg & A. Collins, Baby Boomers: Issues and Trends Summary Analysis Including Opportunities for the Aging Network, National Association of Area Agencies on Aging.
[4] Transitioning into Retirement, The MetLife Study of Baby Boomers at 65 (April 2012).
[5] P. Berg & A. Collins, Baby Boomers: Issues and Trends Summary Analysis Including Opportunities for the Aging Network, National Association of Area Agencies on Aging.
The post BABY BOOMERS AND RETIREMENT first appeared on SEONewsWire.net.]]>There are a large number of agents out there that have issues with using lead generation companies and investing their hard-earned marketing dollars in buying leads. Those same cautious individuals end up watching the competition soar like an eagle when it comes to selling Medicare supplements.
“Why is the competition doing better than you are? They are buying exclusive Medicare supplement leads from benepath.net,” explains Clelland Green, RHU, CEO, benepath.net. “The fact is the Medicare supplement market is ripe for harvesting because the buyers in that demographic need what you are selling. It doesn’t get any easier than that.”
Selling insurance, no matter what kind, is not a walk in the park. Agents should always work their leads, even Medicare leads, with enthusiasm, drive, integrity and determination. The greying of America means there are millions of potential customers to approach with a much sought after health product, one that they need to be as healthy as possible.
The nation’s population is not the only thing aging. So is the Medicare program itself. Some predict it is going to run out of money by 2017. Others suggest it is likely to remain operating, but at a 20 percent less capacity. “That aside, and most such predictions like this need to be taken with a grain of salt,” adds Green. “Medicare supplements help fill the gaps left in health insurance coverage in the ‘original’ Medicare.”
Also referred to as Medigap, Medicare supplements give seniors a better, more complete plan to see them through their medical issues. This point, perfect for educating potential senior customers, may be used in discussion with Medicare supplement leads. Working this type of lead is not just about selling. It is also about education, assisting the client to choose what is the best coverage for their situation and about making someone’s life better.
“With all those points working in your favor, your business can and will grow by leaps and bounds. When you market what people want and need and do a good job of it, they convert. Don’t eschew buying from a lead generation company until you have actually tried it,” Green suggests. “The results will surprise you.”
Medicare supplement leads are a bit like the pot of gold at the end of the rainbow. “Believe in the process and product and reap the rewards,” says Green.
The post Medicare Supplement Leads Are Gold first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., Esquire, CELA
When a defendant causes the death of another individual by a wrongful act or negligence, that person shall be liable for damages. There are two components of the claim. One is a Survival Claim, and the other is the Wrongful Death Claim. The Survival Claim is brought by the estate, either by the executor under a will or the administrator, if the decedent died intestate. For monies received under the Survival Claim, there is usually some confusion about who is entitled to the damages payable to the estate. Generally, the monies are paid to the individuals who would inherit under the New Jersey Intestate statute. This means that the surviving spouse would take 100%. However, there is an exception, if the decedent is survived by a surviving spouse and one or more surviving decedents. In this case, they are entitled to equal proportions for purposes of recovery, notwithstanding the New Jersey Intestacy statute. So, if they are a family with a surviving spouse and three children, each claimant would take 25%.
Under the Wrongful Death Claim, the court allocates damages in such a way to result in a fair and equitable apportionment among claimants, taking into account the age of the dependents, their physical and mental condition, the necessity or desirability of providing them with educational facilities, their financial condition, and the availability to them of other means of support, present and future, and any other relevant factors that will contribute to a fair and equitable portion of the amount recovered.
A major issue is how much should be allocated to the Survival Claim and how much to the Wrongful Death Claim. In many cases, one consideration is New Jersey estate tax and, in some cases, federal estate tax is an issue. Occasionally, New Jersey inheritance tax must also be considered. If the Survival Claim exceeds $5,430,000 in 2015, it is subject to federal estate tax. If the Survival Claim exceeds $675,000, it is subject to New Jersey estate tax. If the beneficiaries of the estate are not blood relatives of the decedent, there will be New Jersey inheritance tax. Monies allocated to the Wrongful Death Claim are not subject to federal or state estate taxes or inheritance taxes. Neither the Survival Claim nor the Wrongful Death Claim are subject to federal or state income taxes.
The second issue is Medicare, Medicaid, ERISA and other liens. Liens would attach to the Survival Claim, but not to the Wrongful Death Claim.
The post SETTLEMENT ALLOCATION IN NEW JERSEY WRONGFUL DEATH CASES first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., Esquire, CELA
In any recovery involving a personal injury case, the interest of Medicare must be considered.[1] The idea is that because Medicare is a secondary payer, a beneficiary should not be permitted to receive a recovery for future medical care, pocket the money, and then bill Medicare for that future medical care.
Are MSAs Appropriate in TPL Cases?
A Medicare Set-Aside Arrangement (MSA) is never required. In the context of Workers’ Compensation (WC) settlements it is a safe harbor. It should be a safe harbor in the context of Third Party Liability (TPL) settlements as well.
In June 2012, The Centers for Medicare and Medicaid Services (CMS) issued a Notice of Proposed Rulemaking.[2] The rulemaking would outline procedures for MSAs in TPL cases. The Office of Management and Budget (OMB) did not approve the proposed rule and CMS withdrew it on October 8, 2014.[3] That leaves practitioners in the same place they were in prior to October 8, 2014. The personal injury attorney, therefore, has five alternatives to consider with respect to an MSA:
- Do nothing to protect Medicare and assume the risk that the rules will be enforced in his case, his client will be denied Medicare coverage for future medicals and possibly bring a malpractice action against the attorney;
- Do nothing but draft releases documenting that the plaintiff has been advised of Medicare’s possible interest and that he knowingly agrees to assume any risk;
- Be prepared to show that Medicare’s interest has been protected by shifting the primary payer – such as a continuing health insurance policy – and assume the risk that the health insurance policy will remain in place and that the person primarily being covered by the policy will not lose his job, die, retire, or become disabled;
- Prepare an allocation report, but do not submit to CMS for approval, and fund the MSA;
- Prepare and submit the MSA to CMS for approval.
The author recommends the fourth alternative to avoid any risk.
[1] 42 U.S.C. §1395y(b)(2).
[2] 42 C.F.R. Parts 405 and 411; 77 Fed. Reg. 35917-35921 (Jun. 15, 2012).
[3] RIN: 0938-AR43 EO 12866 Meetings.
The post WRAPPING A MEDICARE SET-ASIDE ARRANGEMENT INSIDE A SPECIAL NEEDS TRUST first appeared on SEONewsWire.net.]]>The post Changes in Medicare Advantage Plans first appeared on SEONewsWire.net.]]>Medicare Advantage plans are used by more than 16 million elderly and disabled people. The system, an alternative to traditional Medicare, allows private insurers to manage health care benefits.
Reimbursement rates for insurers are announced by the government each April, allowing health insurance companies to plan which options to provide and in which areas to compete. The increase comes after…
by Thomas D. Begley, Jr., Esquire, CELA
In any recovery involving a personal injury case, the interest of Medicare must be considered.[1]
Reasons Support the Argument that the Medicare Secondary Payer Act Applies to TPL Cases with Respect to MSAs
There are a number of reasons to believe that MSAs are appropriate in personal injury cases. They are as follows:
- An informal survey of the 10 CMS Regional Offices by members of the Special Needs Alliance confirmed that each Region has taken the position that even in third party liability (TPL) cases, Medicare’s interests must be considered, and in the absence of further guidance, the Worker’s Compensation (WC) guidelines should be followed.
- The Medicare Secondary Payer Manual now includes language referring to “Liability Set-Aside Arrangement.”
- CMS has issued a memorandum that in TPL cases an MSA is not required “where the beneficiary’s treating physician certifies in writing that treatment for the alleged injury relating to the liability insurance (including self-insurance) ‘settlement’ has been completed as of the date of ‘settlement’ and where future medical items and/or services for that injury will not be required, Medicare considers its interests, with respect to future medicals, for that particular ‘settlement’ satisfied.”[2] The converse would appear to be that if the treating physician will not sign such an opinion letter, the MSA would be required.
- The U.S. Attorney for the Western District of New York has issued a protocol indicating that, under certain circumstances, his office will review MSAs in TPL cases.[3]
- A U.S. District Court[4] has found that a set-aside for future medical expenses in a liability case is appropriate.
Cases Where an MSA is Not Required
There are several situations in which an MSA is unnecessary:
- The facts demonstrate that the claimant is only being compensated for past medicals and not for future medicals. There is no evidence of an attempt to maximize other aspects of the settlement.
- The treating physician concludes in writing that, to a reasonable degree of medical certainty, the individual no longer requires any Medicare-covered treatments related to the claim.
- The client is not receiving Medicare and has no reasonable expectation of receiving Medicare within 30 months. The Medicare Secondary Payer Act does not apply to individuals not covered by Medicare.
[1] 42 U.S.C. §1395y(b)(2).
[2] CMS Memorandum, Subject: Medicare Secondary Payer – Liability Insurance (including self-insurance) Settlements, Judgments, Awards, or Other Payments for Future Medical Information, from Acting Director Financial Services Group to Consortium Administrator of Financial Management and Fee for Services Operations (Sept. 29, 2011).
[3] Western District of New York, Medicare Secondary Payer Protocol, Assistant U.S. Attorney Robert G. Trusiak (May 6, 2011).
[4] Big R Towing, Inc. v. Benoit, 211 W.L. 43219 (W.D. La. Jan. 5, 2011).
The post WHEN IS A MEDICARE SET-ASIDE ARRANGEMENT (MSA) REQUIRED IN A THIRD PARTY LIABILITY CASE? first appeared on SEONewsWire.net.]]>
A continuing care retirement community is able to offer progressive levels of care as they become necessary.
In today’s uncertain economic times marked by roller-coaster markets and flat-line wages, leave it to a certain segment of Michigan seniors and retirees who are choosing to live in bigger homes instead of taking a more common route of downsizing during their retirement years.
In fact, according to a recent report by Merrill Lynch and Age Wave, 49% of retirees in their survey chose not to downsize in “their last move.” Moreover, 30% were electing to move into a much larger home. Such choices obviously belong to a retirement sector quite “confident with their investments.”
More importantly, the survey revealed that about 20% selected a larger home not only to accommodate family visits, but also to provide the space for families to live with them in the future—the survey indicates that 16% of the retirees responding actually had a boomerang child living with them.
Accompanying this ongoing trend is the notion that a larger home may actually provide better in-home care options; this, even though larger homes bring higher taxes, maintenance and even association fees.
Still, and while larger homes can make in-home care a more viable option, the increase interest in other choices, such as assisted living and even nursing home options continues unabated.
Staying in the home.
It may not be surprising that around 90% of seniors polled by AARP showed a preference for ‘aging in place, or staying in their home after the age of 65. Often, that might mean customizing rooms by adding ramps, or installing stairlifts, or even moving an upper bedroom to the first floor.
But when health conditions deteriorate for those ‘aging in place,’ seniors can still receive hospice care in their homes during those end-of-life stages—funded by Medicare and Medicaid services.
Is ‘assisted living’ covered by Medicare/Medicaid?
Of course, the home may not be a viable option, because of expense and minor health issues. As such seniors may favor an assisted living facility. Unfortunately, neither Medicare and Medicaid will pick up room-or-board costs.
However, these facilities accept seniors who may be at different ‘tiers’ of medical need, thereby affecting the resident’s monthly charges. Generally, the more ambulatory you are, the cheaper the overall costs.
By law, these facilities can only offer extra care up to a certain level; then, other options may have to be considered. But if you are fortunate to have long-term care insurance, the policy may provide some “in-home” help while you are in an assisted-living setting.
Continuing Care Retirement Facilities (CCRCs)
Generally, these facilities require a one-time ‘entry fee’, and then monthly payments that reflect the range of services and amenities offered. Ideally, as their ability to live independently decreases, seniors are able to receive progressive care at the CCRC—a viable solution to the universal question of how to avoid nursing home costs.
CCRCs are normally set up to provide around-the-clock care when needed. Of course, with this level of assistance comes higher monthly costs.
‘Assistance’ from your 401(k).
Congress tried to include long-term care (LTC) for all U.S. citizens in the Affordable Care Act (ACA), but it was axed. Instead, the hope is that the IRS will eventually allow us to use our 401(k) to at least pay for LTC premiums, thereby lessening the agency’s current definition of “hardship” cases.
IRS’s existing hardship withdrawal rules do provide for tax-free withdrawals to cover what is considered to be “significant medical expenses.” But it remains questionable that the hardship rules will change; this, owing to the potential decrease in tax revenues that could result.
To start the conversation about the importance of an overall estate plan, including the need for long-term health coverage, contact us today.
The post How to avoid nursing home costs: CCRCs may provide the progressive care needed. appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post How to avoid nursing home costs: CCRCs may provide the progressive care needed. first appeared on SEONewsWire.net.]]>
Though Baby Boomers do focus on cash flow in retirement, planning beyond that with an estate plan is often not on their radar.
Modern medicine is still researching better treatments for Alzheimer’s disease. In the meantime, Congress is considering a different kind of remedy – the law. The Health Outcomes, Planning, and Education, or HOPE for Alzheimer’s Act, was recently introduced into Congress to fill some of the coverage gaps left by Medicare. While Medicare covers the diagnosis of Alzheimer’s disease, it leaves out the lengthy and complex planning for the care that the disease requires. The proposed law would expand Medicare coverage, introducing a benefit that provides caregivers information about the resources available to them as they plan for caring for a loved one who has the disease.
“Current coverage for care planning falls short of what is necessary for people newly diagnosed with Alzheimer’s and their families to adequately process and plan for their new reality,” Robert Egge, chief public policy officer of the Alzheimer’s Association said following the introduction of the bill. “This legislation encourages doctors to talk to their patients about an Alzheimer’s diagnosis and ensures that the necessary steps are taken to provide them with access to available care planning services.”
Alzheimer’s Effects Many Michigan Seniors
According to figures from the Alzheimer’s Association, more than 5 million American are currently living with Alzheimer’s disease, which is the sixth leading cause of death in the United States, killing an estimated 500,000 people each year. But the association also says that nearly half of people with Alzheimer’s disease, or their caregivers, say they were not told of the diagnosis by their doctor. That’s a stark contrast to cancer. In the four most common types of cancer, more than 90 percent of people were told of their diagnosis, the Alzheimer’s Association’s says.
Even when patients or their caregivers receive the Alzheimer’s diagnosis from their doctors, they are more likely told only after the disease has already reached a more advanced stage. Why are doctors not forthcoming with such important diagnostic information? According to an Alzheimer’s Association survey, it’s because doctors believe that there’s nothing that can be done about the disease.
Alzheimer’s Consequences
Unfortunately, a late Alzheimer’s diagnosis has consequences. The absence of a diagnosis from the medical record could adversely impact how caregivers coordinate care and manage any chronic conditions. That’s important because complications from managing chronic conditions increases health care costs, the Alzheimer’s Association says. Alzheimer’s and other dementias are already expensive diseases on their own, costing a projected $226 billion in 2015. By 2050, the association projects that those costs rise to $1.1 trillion. The inability to properly coordinate care because of a late Alzheimer’s diagnosis will only compound those costs.
The association points to studies showing that early diagnosis comes with benefits. For example, an early diagnosis means patients still have the ability to be an active part of the planning for their care. Early diagnosis also enables a person to choose to participate in support services or clinical trials, if those are desired options.
HOPE for Alzheimer’s has bipartisan support. Introduced by lead sponsor Sen. Debbie Stabenow, a Michigan Democrat, it is co-sponsored by Sen. Susan Collins, a Maine Republican. In the House of Representatives, the legislation is sponsored by New Jersey Rep. Chris Smith, a Republican, and Rep. Paul Tonko, a New York Democrat.
If passed into law, HOPE for Alzheimer’s would put the burden on the Department of Health and Human Services to conduct outreach to inform health care providers about the services under the new law. It would also require HHS to report on any barriers that people encounter in accessing services, and then provide recommendations to overcome them.
“This is very much a family disease, because the whole family is impacted by this, so we need to take the next step,” Stabenow told Michigan Radio. “Make sure that people are getting diagnosed, that they know what’s available, and that we can start the process of supporting the family.”
To learn more about what the HOPE for Alzheimer’s Act could mean for you and your family, contact us.
The post Alzheimer’s Patients, Caregivers Receive “HOPE” Under Proposed Alzheimer’s Law appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Alzheimer’s Patients, Caregivers Receive “HOPE” Under Proposed Alzheimer’s Law first appeared on SEONewsWire.net.]]>
The HOPE for Alzheimer’s Act is designed to fill coverage gaps left by Medicare, and encourages doctors to help their patients plan for the long-term care the disease requires
Alzheimer’s disease is a serious medical condition that affects a persons cognitive functions. There are often personality changes, loss of bodily functions and memory issues which causes difficulty with daily activities. It often occurs with the elderly, but also happens to younger people, called early onset. It’s one of the most common illnesses in the senior population.
Alzheimer’s Disease Stages
Alzheimer’s goes from mild stages to more severe stages over a course of time. More serious medical problems occur because the body loses important functions like feeding, using the bathroom and loss of independence.
There are three stages of Alzheimer’s disease. In the early stage, the patient still functions independently, but they begin to lose their cognition. The mid-stage is when they are semi-dependent on the caregiver and have memory and self-identity problems with personality changes. The late stage is severe and they are fully dependent on the caregiver. The disease is highly progressive.
Patients with Alzheimer’s begin to misplace common, important things. They will start having issues with talking and remembering their own native language. They begin to lose memory, causing them to forget or even become unable to recognize family members. They will lose their happiness, patience, or desire for things that they used to enjoy doing. Their judgment skills will become non-existent. Patients will forget life skills, such as cooking, dressing and doing familiar tasks.
Signs and Symptoms of Alzheimer’s
Signs and symptoms of Alzheimer’s include:
- Confusion and disorientation
- Socially inappropriate behavior
- Depression, anxiety and irritability,
- Lack of judgment and abstract thinking
- Paranoia
People with Alzheimer’s have understandable issues with accepting their disease. They may blame others or deny it. This is frustrating for all concerned. The person deserves proper treatment, with love, respect, patience and kindness.
During the middle stage of Alzheimer’s, the patient will start to forget who they are and all the things that they used to do. The person usually lives from 3-20 years after diagnosis. They will require help from a caregiver which is costly. They will need a loved one to help plan things out financially for them.
Full-time care is important in the late stages. During this time, the patient needs help with using the restroom and eating because they will forget to do these things alone. Their body is unable to do so automatically anymore. This is upsetting for the family. Caregiver stress is common. Asking for help from others is an important part of the entire plan for their care.
When caring for someone with Alzheimer’s, tell them when its time for an activity. Always explain what you are doing slowly and carefully so they have a better chance of understanding. Even if this seems silly to you, keep in mind that they are having trouble remembering. The unknown is frightening and causes negative behaviors to develop. If they refuse care, make sure it isn’t because they don’t understand you. If they insist on fighting you every step of the way, take a deep breath, walk away and try again at a later time.
The Debilitating Effect of Alzheimer’s Disease for Michigan Seniors
Alzheimer’s disease is one of the most debilitating diseases. It is sadly very common and there is no known cure. Although Alzheimer’s cannot kill the body directly, it does basically destroy the brain, the control center of all bodily functions. When a persons vital body organs malfunctions, then the person will eventually pass away.
There are medications that help slow down the symptoms of the disease. A medication called Donepezil blocks certain enzymes, which is widely used in hospitals and nursing homes for this reason. There are many other medications which work on the same principles using different scientific ideas.
Currently, there is plenty of research going on for the cure of Alzheimer’s disease. If you’d like more information, please contact us.
The post Understanding Alzheimer’s and Caring for a Loved One appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Understanding Alzheimer’s and Caring for a Loved One first appeared on SEONewsWire.net.]]>

Before the House adjourned for a two-week recess, representatives passed legislation overhauling the outdated method for paying physicians who accept Medicare. Physicians and seniors across America are breathing a sigh of relief, as the bill ensures access to better healthcare services and professionals, many of which quit treating Medicare patients altogether due to the dysfunctional Sustainable Growth Rate Formula (SGR) implemented in 1997. 
Here are the highlights of the bill:
- The legislation replaces the current model of paying physicians based on the services provided (also known as ‘fee-for-service’) to value or outcome based payment (‘fee-for-value’);
- The popular Children’s Health Insurance Program (CHIP), which provides health care coverage for low-income children was extended for another two years; and
- The bill requires seniors who make more than $133,500 to pay more for Medicare coverage starting in 2018.
Although the bill will add $141 billion to deficit over a decade, the bill promotes higher quality of care for Medicare patients and long-term sustainability of the Medicare program. The House passed the bill in an overwhelming bipartisan vote of 392-37. Now the U.S. Senate must pass the bill when Congress reconvenes April 13.
Learn more about our services by visiting www.littmankrooks.com.
Was this article of interest to you? If so, please LIKE our Facebook Page by clicking here.
The post Bill Overhauling Medicare Passes in the House first appeared on SEONewsWire.net.]]>How Are Ratings Calculated?
Nursing homes are graded in three ways. First, trained surveyors perform inspections on site. These include annual inspections and those prompted by a complaint. Second, specific quality measures are assessed. Eleven quality measures are scored based on clinical data reported by the nursing home themselves. Lastly, the staffing of the home influences their grade. While the federal government requires enough staffing to adequately care for residents, there is no specific ratio. Therefore, the CMS staffing rating is the only existing guideline currently. Staffing is calculated by Registered Nurse (RN) hours per resident day and total staffing hours per resident day, including RNs, Licensed Practical Nurses (LPN), Licensed Vocational Nurses (LVN) and Certified Nurses Aids (CNA). By going to the Nursing Home Compare website, users can look at overall ratings or view how each home scores in these three categories separately. While the rating system was launched in 2008, two new factors are being considered in their quality measurements.
- Antipsychotics. Homes will be rated on their use of antipsychotics. Research has shown that homes often prescribe these medications for conditions that do not require them. Now, they will be scored by how much they use antipsychotics on long-term and short-term patients.
- Staffing. CMS has updated how much staffing influences a home’s overall score. Nursing homes must now earn four stars in their total staffing or RN rating to get at least an overall four-star rating.
CMS Warns of Initial Decline
Before the recent revisions, about 80 percent of homes received a four or five-star rating. CMS estimates now only about 49 percent will get these high ratings. About two-thirds will see a drop in their quality ratings and one-third will see decline in their overall score. However, CMS is confident the scores will increase as nursing homes work hard to make improvements in line with the quality of care reflected by the scoring process. In fact, benefits are already being seen. For example, CMS has been focusing on reducing the amount of antipsychotics for the last couple years. By the end of 2013, there was a 15 percent reduction compared to 2011. In coordination with the National Partnership to Improve Dementia Care, CMS has set a goal to reduce antipsychotic use by 30 percent by the end of 2016.
Selecting a Home
While Nursing Home Compare is extremely helpful, selecting a home for your loved one requires much more than viewing a rating system. Many factors much be considered, including proximity to family, amenities, quality of life offered, treatment required by the patient, costs and numerous other factors. An on site visit and interview with staff will help you get a feel for the atmosphere. While comfort and quality are your top priority, cost cannot be ignored either. Families must consider not only the out-of-pocket costs, but also a strategy to protect your loved one’s assets. An experienced Medicaid attorney can help protect your assets, as well as determine what coverage you qualify for. Talk to an attorney at The Elder Care Firm about the use of trusts, transferring assets, purchasing annuities or a strategy that increases income and resource allowances for family members. Contact us to get started.
The post Medicaid Updates Nursing Home Ratings, Helping to Make Long-Term Care Decisions Easier appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Medicaid Updates Nursing Home Ratings, Helping to Make Long-Term Care Decisions Easier first appeared on SEONewsWire.net.]]> When it’s time to arrange long-term elder care for a loved one, you’ll be facing a taxing time full of stress and expense, on top of all you are already going through. Which has potential to be even more challenging when your loved one requires specialized care, needs a full-time nurse, or has some other form of care that costs money that may not have. The fact is, assisted living costs are exorbitant, and the money you spend giving aid to your loved one is on the rise.
When it’s time to arrange long-term elder care for a loved one, you’ll be facing a taxing time full of stress and expense, on top of all you are already going through. Which has potential to be even more challenging when your loved one requires specialized care, needs a full-time nurse, or has some other form of care that costs money that may not have. The fact is, assisted living costs are exorbitant, and the money you spend giving aid to your loved one is on the rise.
According to assistedliving.com, 70% of all people over the age of 65 will need some type of long-term care. Additionally, costs are on th increase. In 2012, a survey found that the average monthly rent for a person receiving long-term care increased by $100 from previous year. If this trend continues over the next decade, what was once a stressful situation has the potential to turn into an unbeatable monster.
So while setting up assisted living for someone you love may seem like a battle you can’t win, now’s not the time to give up hope. There are several strategies, that a person on any type of budget can implement to help offset assisted living costs. Here are just 7.
7 Strategies to Reduce Assisted Living Costs
1. Research is a golden ticket. As much as most people would like for the a situation like this to work itself out, that’s simply not going to happen. Research opportunities, before the time arise, as a preemptive measure, and you’ll see how much easer the process ends up.
2. Start saving money now. If you are reading this, then you likely have a loved one who will need assisted living at some point soon. If so, start squirreling money away ASAP. Every little bit you put away has more power than you can imagine, especially when money is tight later down the road.
3. One and done, with care. If you have to re-home a loved one after already placing them in assisted living, you are essentially adding unnecessary costs. To avoid this, don’t be afraid to ask the tough questions from the start; ask people who work for the company about the standards, check licenses and names, and have your attorney review the living contract. Your loved one is worth the extra time.
4. Negotiations work. Many assisted living companies offer incentives (just like any business), for new patients. Before you agree to any arrangement, inquire about perks that may reduce your monthly payments. You’ll be surprised at how much people will want to work with you.
5. Keep a broad eye out. If you exhaust your resources in the area you live in, branch out. You may be surprised at the resources in neighboring communities and cities. Use your time to take a closer look into other opportunities, and consider an alternate locale.
6. Insurance may work in some situations. Assisted living, as we noted above, is expensive in any situation. For those who are on a tight budget, perhaps it’s time to consider insurance options, beginning with Medicaid or Medicare. While these government programs are a good start, they don’t always pay for everything. So take a look at some additional insurance programs to help offset what they lack.
7. Discuss the types of care you require. Not every person who needs assisted living needs the same care. Some people only need assisted living, as opposed to being moved into a facility. When deciding what will work best for your loved one, it’s important to place value on what they truly need. Expenses related to living at home, versus general assisted living costs, are particularly relevant to those on a budget.
If all else fails, then perhaps it’s time to speak a care advisor about your particular needs. A knowledgeable person who spends a majority of their time assisting our elders might be your ticket to long-term savings, while giving the care your loved one deserves.
For more information on how we can help you through this difficult time, please don’t hesitate to contact us to discuss your options.
The post 7 Helpful Tips to Reduce Assisted Living Costs appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post 7 Helpful Tips to Reduce Assisted Living Costs first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
This article continues the discussion of special problems for the elderly. (Here is a link to Part 1.)
- Long-Term Care. About 70% of Americans will require some form of long-term care be it home care at $22 to $25 per hour, assisted living at $4,500 to $8,500 per month, or nursing homes at $10,000 to $12,000 per month. Only about 6% to 8% of Americans have long-term care insurance. Expenses of long-term care will wipe out most families very quickly. The Affordable Care Act has already covered between 10 and 13 million additional individuals. That number would be much larger except that 22 states refuse to expand Medicaid eligibility to their states. The Affordable Care Act, or Obamacare, was merely not health reform, it was insurance reform. Much of the legislation was designed to protect insurance companies. A better solution would have been a single payer health care system. This would have been much more efficient for doctors, hospitals, and other health care providers. Essentially, it would be Medicare for everybody. Individuals would still have the right to choose their own health care providers, but all bills would be paid by an agency of the federal government. The federal government would not control the care, simply the payment. Another factor contributing to rising health costs is that the federal government is not allowed to negotiate prices with pharmaceutical companies under Medicare Part D. Other agencies of the federal government, such as the Veterans Administration, are able to negotiate prices and receive significant discounts.
- Transportation poses special problems for senior citizens living in the suburbs. The suburban lifestyle is based on the automobile, and once the elderly can no longer drive, their ability to live independently is curtailed by a lack of public transportation in suburban and rural areas. Public policy should favor the development of multi-modal transportation systems that are highly inter-connected.
- Housing is the largest category of consumer expenditures for households age 65 and older. Expenditures for age 65 years and older break down as follows:[1]
Housing 36.7%
Transportation 13.34%
Food 12.44%
Health Care 14.74%
Cash Contributions 7.9%
Entertainment 18.84%
[1] The Bureau of Labor Statistics Consumer Expenditures in 2012, www.bls.gov.
The post SPECIAL PROBLEMS AFFECTING THE ELDERLY – PART 2 first appeared on SEONewsWire.net.]]>In lockstep with good content, make the design of the email interesting, eyecatching and yes, relevant to your audience. If you are creative enough, your mailing list of existing and prospective customers start to look forward to what is coming next. While you may not achieve a 100 percent open rate, you could come pretty close by being a smart email marketer.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Other things to avoid in email marketing campaigns first appeared on SEONewsWire.net.]]>by Thomas D. Begley, Jr., CELA
As the population of the United States tend to age and Baby Boomers begin retiring in large numbers, there are a number of problems that will affect the elderly that need to be addressed.
- Retirement Income. In 2012, people age 65 and older had an average income of $31,742, but the median income was less than $19, 604. About 30% of older Americans receive pensions. The median was $12,000. Only 46.5% of older Americans reported income from personal savings, but half receive $255 or less per year. The mean was $3,233 per year. Only 20% of older Americans had dividend income with the median amount being $1,200.[1] Social Security is the only source of income for 25% of older adults in New Jersey.[2] It is generally estimated that for a comfortable retirement a person must have an income equal to 70% of salary in the year just before retirement. Most experts advise saving 10% per year of one’s annual income beginning at age 25. Social Security plays a vital role in reducing poverty. Almost 90% of people age 65 or older receive some of their family income from Social Security. The Social Security Retirement System is expected to be able to pay full benefits through 2033. Thereafter, only 75% of benefits will be funded. The Disability Insurance Trust Fund paying disability benefits to disabled workers is expected to be solvent through only 2016, at which point only 81% of benefits can be funded. This problem has been discussed nationally for over 20 years, and Congress has always managed to dodge the hard decisions. The replacement of pensions with 401k plans has been disastrous for low-income workers. Workers in the top fifth in income account for 72% of total savings in retirement accounts.
- Health Care. Health care spending has increased significantly. While this spending has declined over the last three years, the Brookings Institute believes that health care will continue to grow 1.2% faster than GDP over the next 20 years and will consume close to 25% of GDP. Health care costs will continue to grow at GDP plus 1.2% for the foreseeable future.[3] A couple, both age 65 in 2012, living an average life expectancy, could need as much as $220,000 to cover premiums for health insurance coverage and out-of-pocket expenses during retirement. It is estimated that these households should expect medical bills to consume 61% of their Social Security payments by 2027.[4]
Medicare. Medicare covers only about one-half of retiree health expenses. Medicare has three components: Hospital Insurance (HI) or Medicare Part A; Supplemental Medical Insurance (SMI) consisting of Medicare Part B and Part D. The SMI program is not threatened with insolvency, because premiums are reset on an annual basis based on actual expenditures. The Trustees of the Federal Hospital Insurance Fund estimate that the HI Program can remain solvent until 2030. Again, this is a problem that has been discussed nationally for over 20 years and Congress has refused to m
[1] Sources of Income for Older Americans 2012, Ke Bin Wu, AARP Public Policy Institute, www.aarp.org.
[2] The Elder Economic Security Standard Index for New Jersey.
[3] Brookings Papers on Economic Activity, www.brookings.edu.
[4] Fidelity Estimates Couples Retiring in 2013 Will Need $220,000 to Pay Medical Expenses Throughout Retirement, www.fidelity.com.
The post SPECIAL PROBLEMS AFFECTING THE ELDERLY – PART 1 first appeared on SEONewsWire.net.]]>But both VA itself and most experts strongly urge veterans to enroll in Medicare. One of the most compelling reasons, cited by Stan Hinden in an article for AARP, is that VA medical coverage is funded by an appropriation from Congress that must be passed each year. As a result, VA does not guarantee benefits in the future, because funding levels may not be sufficient to cover the needs of all veterans. The National Council on Aging agrees that the priorities and funding of VA can change, and that veterans could see the VA benefits they have now decrease in the future.
Veterans who sign up for Medicare will have health coverage for a wider array of medical services, and they will be able to access private doctors and medical facilities. This can become especially important as veterans age and encounter more complex health concerns.
Medicare can also provide vitally necessary coverage in urgent situations. For example, if a veteran is taken to a non-VA hospital ER, Medicare will cover the costs of care. Or, if a veteran is pre-authorized by VA for treatment in a non-VA hospital, Medicare may pay for additional treatments that become necessary but were not expressly authorized by VA.
Low-income veterans may be especially concerned about the cost of Medicare premiums. But Medicare premium assistance programs are available to low-income individuals, including veterans. In Michigan, the Michigan Department of Community Health runs the program that provides premium assistance to Medicare recipients.
Finally, veterans should be aware that Medicare imposes penalties on individuals who sign up after the initial enrollment period. Typically, to avoid penalties, individuals must sign up for Medicare in a seven-month window surrounding their 65th birthday. Individuals who fail to do so, including veterans, will pay higher premiums if they decide to sign up later.
The National Council on Aging offers more information on Medicare for veterans with VA benefits on the website mymedicarematters.org. In addition, many veterans benefits attorneys offer assistance to veterans seeking all of the coverage to which they are entitled.
Legal Help for Veterans, PLLC fights for veterans rights. We fight to make sure you get the benefits you deserve from the Department of Veterans Affairs. To learn more or contact a veterans lawyer, visit http://www.legalhelpforveterans.com/ or call 800.693.4800
The post Veterans Should Sign Up for Medicare When Eligible, Even With Good VA Benefits first appeared on SEONewsWire.net.]]>Timing is everything when it comes to marketing a product, and that is especially applicable for the insurance industry. Marketing Medicare to a 20 year old just does not work as well as marketing to those a few years short of 65-year-old, and for them you are often marketing Medicare supplements to, well, supplement the holes in the original Medicare insurance.
Know your product. Know when to market it. Know who to market it to, and your agency is bound to attract customers in large numbers.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Does social media help when it comes to marketing insurance articles? first appeared on SEONewsWire.net.]]>By Thomas D. Begley Jr.
WHAT SHOULD YOU KNOW ABOUT LONG-TERM CARE?
Long-term care is an area of growing concern to older Americans and their families. Approximately 70% of individuals age 65 or older eventually require some form of long-term care. Whether that consists of home healthcare, assisted living or nursing home care, the costs can be substantial. Without adequate planning, long-term care costs can quickly deplete a lifetime of savings. That, in turn, can jeopardize the financial security of a surviving spouse and undo any plans for transferring wealth to children.
Given the complexity of long-term care planning and the potential for costly errors, it is important to retain an experienced Elder Law attorney to guide you through the process.
HOW CAN YOU PLAN FOR LONG-TERM CARE NEEDS?
Generally, the long-term care planning process involves:
- Identifying and prioritizing goals.
- Tax planning.
- Considering funding alternatives.
- Choosing appropriate planning tools.
- Applying for Medicaid, as necessary.
WHAT ARE YOUR GOALS?
The first step in long-term care planning is identifying goals and priorities. Typically, individuals want to:
- Obtain the best quality of care for the person in need.
- Maintain financial security for the healthy spouse.
- Avoid becoming a burden on children.
- Preserve a legacy for children.
- Avoid Medicaid lien on homes.
- Understand and plan appropriately for taxes, including:
- Income tax.
- Gift tax.
- Federal estate tax.
- New Jersey estate tax.
- New Jersey inheritance tax.
- Capital Gains tax.
WHAT SHOULD YOU KNOW ABOUT TAX PLANNING?
As you consider which assets might be used to fund long-term care and which you would like to leave to your children, it is important to understand the income tax ramifications of the following:
- Medical deductions. It is possible to take a medical deduction for qualified long-term care costs. For nursing home care, the deduction usually is equal to 100% of the cost of care. For assisted living and home care, it usually is a portion of the cost of care.
- Carryover basis. If a parent transfers assets to a child, the parent’s cost, known as the basis, carries over to the child, becoming his or her cost basis. This exposes the child to substantial capital gains taxes when the asset is sold.
- Step up in basis. If a parent leaves a child an asset that has increased in value, the child’s cost basis “steps up” to the fair market value of the asset at the parent’s death. This saves the child a significant capital gains tax bill when the asset is sold.
- Retirement plans. The tax treatment of qualified retirement plan assets makes them a good source of funding for long-term care, if funds are needed. While distributions are taxable (since the funds have grown on a tax-deferred basis while in the account), taxes are at least partially offset by the medical deduction, provided the funds are used for long-term care. Since there is no step up in basis on these assets, passing them to children would have capital gains as well as ordinary income tax consequences.
- Deferred annuities. Annuities in which the income has been deferred provide another good source of long-term care funding. When the income is withdrawn, it is taxable at ordinary income tax rates. But those taxes can be at least partially offset by the medical deduction if income is used for long-term care. If the annuity is transferred to a child; however, the entire deferred income is immediately taxable, and there is no step up in basis.
- Interest on E, EE, H, and I bonds. Long-term care costs also may be funded with these types of bonds. To the extent that the bonds have deferred interest, which has not been taxed, that interest is taxable when the bonds are redeemed. But those taxes can be offset, at least partially, by the medical deduction, as long as the funds are used for long-term care. If these bonds are passed on to children, there is no step up in basis.
- Gain on the sale of a home. As a general rule, if you have resided in a home as your principal residence for two of the five years preceding the date of sale, you are entitled to a $250,000 exclusion from capital gains tax, if single, or a $500,000 exclusion if you are married.
- Capital gains tax. There is a federal capital gains tax levied at the rate of up to 20% on profit from the sale of appreciated assets, such as homes and securities. There is also New Jersey income tax on this profit.
HOW WILL YOU PAY FOR LONG-TERM CARE?
There are five ways to pay for long-term care: private pay, long-term care insurance, Medicare, Veterans Administration benefits, and Medicaid.
Private pay
Paying for long-term care privately is the least desirable option since few families can afford the $100,000+/- annual price tag over an extended period of time.
Long-term care insurance
While long-term care insurance is an excellent way to pay for care, only 6- 8% of the elderly have this type of insurance. There are four reasons people don’t buy long-term care insurance:
- Lack of awareness. The industry has not done an adequate job marketing this product.
- It is estimated that only 10- 20% of the elderly can afford the long-term care insurance.
- At age 65, 25% of long-term care insurance policy applicants are rejected for health reasons.
- Since most people are optimists and prefer not to consider unpleasant outcomes, they don’t think they’ll need it. This proves to be the wrong decision 60% of the time. Unfortunately, the consequences of this mistake can be financially devastating to individuals and their families.
When buying long-term care insurance, it’s important to consider these factors:
- The type of care covered.
- The amount of daily benefits.
- Elimination periods.
- Inflation riders.
- Pre-existing condition clauses.
- The length of coverage.
- Guaranteed renewability.
- Waiver of premiums.
- The financial strength of the insurance company.
Medicare
If you expect to have Medicare cover long-term care costs, you should know that it:
- Offers extremely limited payment for home care and no payment for assisted living.
- Will pay for a nursing home stay only under certain conditions. The patient must have had a Medicare-covered stay in a hospital lasting at least three days and must have entered a nursing home to obtain skilled care within 30 days of discharge from the hospital.
- Will not pay for custodial care. The patient must receive skilled care to qualify for Medicare. If that level of care stops, the Medicare payment will stop. Examples of needs requiring skilled care include insertion of a feeding tube, five day per week rehabilitation, and insulin dependence.
- Will pay for a maximum of 100 days. That amount of coverage is not guaranteed and is a maximum, not a minimum. There is a co-insurance from day 21 through day 100. For 2015, the co-insurance rate is $157.50 per day. That may be covered if the patient has the appropriate Medi-gap policy.
Veterans’ benefits
If you believe you are eligible to have Veterans’ benefits cover long-term care costs, you should be aware of the following:
- Federal VA nursing homes. A veteran whose disability is 70% or more service-related is entitled to free lifetime nursing home coverage, regardless of means. These individuals are given priority for admission to federal VA facilities. Veterans who do not have a service-related disability are means-tested to determine eligibility for payment. As a practical matter, these individuals are unlikely to gain admission to a federal VA facility.
- VA Aid & Attendance benefits. Veterans Aid & Attendance benefits are available to certain veterans. These individuals must have served for at least two years of active duty and one day must have been during a war. There are income and resource eligibility tests. Aid & Attendance is available to veterans and to spouses of deceased veterans. For 2015, the monthly benefit for a veteran with dependents is $2,120, for a single veteran $1,788, and for the spouse of a deceased veteran $1,149.
- State VA benefits. The New Jersey Veterans Administration operates three Old Soldiers’ Homes for New Jersey veterans and their families. They are located in Paramus, Edison and Vineland. Veterans, spouses of veterans, surviving spouses, and, in some cases, parents, may be eligible to enter these facilities. Space is limited, and there is often a long waiting list. The monthly rate for Veterans who are not financially qualified is much lower than that for private nursing homes. Financially-eligible veterans qualify for a subsidy, which further reduces the cost dramatically. In some instances, a spouse remaining at home is entitled to retain a portion of the resident’s income for certain expenses.
Medicaid
If you may need to rely on Medicaid to cover long-term care costs, you should be aware of the following:
- Income limits. For 2015, there is an income cap of $2,199 per month for Medicaid eligibility. However, if an individual’s income exceeds that cap, a Miller Trust can be established to obtain income eligibility. Under a Miller Trust, a portion the Medicaid applicant’s income is deposited into a trust to bring the remaining income under the income cap. This is a legal fiction that makes no sense, but it enables many individuals to obtain Medicaid in nursing homes, assisted living facilities, and at home who would not otherwise be eligible.
- The Minimum Monthly Maintenance Needs Allowance. Medicaid regulations provide that if the applicant is married, the spouse remaining at home is entitled to a minimum monthly allowance. In some situations, if there is a shortfall, the difference can be retained from the income of the spouse requiring care. For the period of July1, 2014, through June 30, 2015, the Minimum Monthly Maintenance Needs Allowance is $1,966.25 and the Excess Shelter Allowance threshold is $589.88 per month for certain housing expenses.
- Resource limits. Persons receiving Medicaid generally can have assets of no more than $2,000. Certain assets are excluded, such as a home (occupied by a community spouse or child who is under age 21, blind or disabled), an automobile, personal effects, prepaid funeral expenses, medical equipment, inaccessible resources (such as an estate in probate), term life insurance, whole life insurance with a maximum face value of $1,500, and a $2,000 personal needs account.
If there is a joint account owned by the applicant “or” another individual, Medicaid takes the position that the entire account is a countable resource for the Medicaid applicant. If the account is owned by the applicant “and” another individual, Medicaid assumes that there was a transfer of assets when the applicant(‘s/s’) child was added to the account, but that each joint owner owns a pro rata share of the account. If the child contributes the assets and later withdraws them, there is no transfer-of-asset penalty. The child bears the burden of proof regarding whether he or she made a contribution to the account.
- Pooling of assets. If a Medicaid applicant is married, the resources of both spouses are pooled to determine Medicaid eligibility. A snapshot of the couple’s resources is taken as the first moment of the first day of the first month in which one of the spouses receives an institutional level of care, even if that care is delivered at home. The well spouse is entitled to a Community Spouse Resource Allowance, but the remaining assets must be spent down prior to Medicaid eligibility.
The Community Spouse Resource Allowance is 1/2 of the countable resources with a maximum of $119,220 and a minimum of $23,844 for 2015.
- Transfer-of-assets rules. Medicaid has strict requirements regarding the transfer of assets from an applicant to his or her children or other parties.
- Medicaid imposes a 60-month (five-year) lookback for transfers of assets. This means that Medicaid will review the applicant’s relevant financial records going back five years to determine whether funds have been transferred during that time period.
- If assets were transferred during the lookback period, Medicaid imposes a penalty. That penalty, which is a period of ineligibility for Medicaid, is calculated by dividing the amount transferred by the average cost of a nursing home in New Jersey determined by the Division of Medical Assistance and Health Services. Unfortunately, this divisor is always less than the actual cost of care.
Penalties may be for a period of months or partial months. The larger the transfer, the longer the period of ineligibility. The penalty does not begin until the applicant is eligible for an institutional level of care, is otherwise financially eligible for Medicaid (i.e. has spent down assets to $2,000) and has no other period of ineligibility outstanding.
For example, assume that a person transferred $50,000 within the lookback period, triggering a seven-month penalty or period of ineligibility for Medicaid. The penalty period would begin when that person was already in a nursing home, had spent down assets to $2,000 and had no other period of ineligibility outstanding. Consequently, the individual would have no money with which to pay for the nursing home care for seven months.
- Acceleration strategies. There are many strategies available to accelerate the date of Medicaid eligibility. These strategies fall into two categories spend down and transfers.
Spend Down. It is possible to spend down assets through:
- Repayment of debt.
- Payment for services.
- Purchase of personal effects.
- Making home improvements.
- Prepayment of funeral expenses.
- Purchase of an automobile for a healthy spouse.
- Purchase of a home for a healthy spouse.
- Purchase of a life estate.
- Establishment of a care agreement.
Transfers. Despite the five-year lookback, in many instances, it is still possible to transfer assets. For example, some transfers are exempt from Medicaid transfer-of-asset penalties. In some cases, tax advantages can be achieved by transferring assets. Additionally, assets may be transferred from one spouse to another through divorce.
Transfer alternatives. There are several ways to transfer assets.
- It is important to consider whether a transfer should be made outright to children or to a trust. Outright transfers have many risks. They can expose assets to the children’s creditors or make them available in a divorce settlement. If grandchildren plan to apply for college financial aid, the transferred assets will need to be disclosed on the application, potentially resulting in a reduction of elimination of aid. Additionally, when assets are transferred to the children, they will lose the step up in basis they would have received if the assets were passed after the parent’s death. The principal residence exclusion on the sale of the home will be lost as well.
If assets are transferred to a grantor trust, the trust can be designed so that, at the parent’s death, the assets will receive a step up in basis. That will result in significant tax savings for the children. The trust also can stipulate that the income tax on the trust assets will be paid by the parent. If a home is transferred to a trust and later sold, the trust can be established to preserve the $250,000 or $500,000 exclusion from capital gains tax on the sale of a principal residence. Additionally, trusts can eliminate risk factors associated with outright transfers to children. Even if a child is serving as trustee, the assets would not be subject to the claims of that child’s creditors or become involved in an action for divorce. These assets would not need to be disclosed on a grandchild’s application for college financial aid.
Several types of trusts are used when Medicaid planning is at issue. All of these trusts are irrevocable.
- Children’s trusts. Assets are transferred to a trust, and the parent does not reserve the right to receive income from those assets. If the parent receives Medicaid and transfers assets out of the trust, there is the risk that there may be a transfer-of-asset penalty. That penalty would be imposed by multiplying the parent’s annual income by his or her life expectancy and dividing the sum by the state divisor.
- Donee trusts. This type of trust is appropriate when a parent transfers assets to children, outright, but the children plan to later establish a trust to hold the transferred assets.
- Disability annuity trusts. If a parent has a disabled child, assets can be transferred to a disability annuity trust for that child’s benefit.
- Disability annuity special needs If a parent has a disabled child who is receiving SSI and Medicaid, assets must be transferred to a disability annuity trust wrapped within a special needs trust in order to preserve the child’s benefits.
Care agreements. In many cases, a child provides care to a parent. To accommodate such an arrangement, the child may move into the parent’s home or the parent may move into the child’s home. Alternatively, the child may provide care while retaining a separate residence from the parent if the parent resides in a nursing home or assisted living facility. It is possible for the parent to compensate the child for this care, effectively transferring assets to the child. This can be done without triggering a penalty, provided that three requirements are met:
- There must be a written care agreement.
- Payment can be made only for care provided after the date of the agreement.
- Compensation must be reasonable.
Note that the income paid to the child is taxable because it is for services. In some circumstances, the parent must withhold from the child for FUTA and FICA. Withholding from income tax is not required unless both parties agree. Medicaid resists these care agreements and great caution must be taken in properly drafting the documents and in delivering appropriate services.
There are several ways to transfer a home.
- Transfer outright to children. A common mistake is for parents to transfer a home outright to children. This results in a number of negative consequences.
- Loss of control. The parent loses control over the home.
- Gift taxes. Since the home is worth more than $14,000, it exceeds the allowable annual exclusion gift.
- Carryover basis. The parent’s cost basis in the home carries over to the children. In some cases, the parent purchased the home many years before, and there has been significant appreciation. Eventually, the children will have to pay capital gains tax on that appreciation.
- Loss of principal residence exclusion. The $250,000/$500,000 principal residence exclusion is lost since the parent no longer owns the home.
- Loss of real estate tax benefits. The homestead tax rebate, Veteran’s deduction, senior citizen’s deduction, tax freeze, and ability to itemize deductions are all lost.
- Transfer, reserving a life estate/right to use or occupy. When the home is transferred to children, but the parent reserves a life estate or right to use and occupy it, the following occur:
- The parent retains control. The children cannot sell or mortgage the house without the parent(‘s/s’) signature on the deed or the mortgage.
- Gift tax exemption. A gift tax exemption can be filed as long as the value of the home does not exceed $5,430,000. In most cases, there will be no taxes due.
- Step up in basis. At the parent(’s/s’) death, the children receive a step up in basis on the value of the home, which reduces their capital gains tax liability.
- Real estate tax benefits. The homestead tax rebate, Veteran’s deduction, senior citizen’s deduction, estate-tax freeze, and ability to itemize deductions on income tax returns are all retained.
- Loss of principal residence exclusion. The principal residence exclusion is lost. This is an important consideration if the home is sold during the parent’s lifetime.
- Transfer to a grantor trust. The home also may be transferred to a grantor trust, with the following outcome:
- Control of the home vests in the trustee rather than the parent.
- Gift tax exclusion. There is no gift tax due when the gift is to a grantor trust.
- Step up in basis. The children receive a step up in basis at the parent(’s/s’) death.
- Loss of real estate tax benefits. The homestead tax rebate, Veteran’s deduction, senior citizen’s deduction, estate tax freeze, and ability to itemize deductions on income-tax returns are all lost.
- Principal residence exclusion. This can be maintained.
- Sell a remainder interest. A parent can sell a child a remainder interest in the home and retain a life estate. It is likely that Medicaid will require the parent to live in the home for one year for this strategy to be effective. The value of the remainder interest is determined by tables published by the federal government. The older the parent, the greater value of the life estate. At age 75, the life estate is worth approximately 52% and the remainder interest is worth approximately 48%. If the parent had a home valued at $200,000, the child would pay approximately $96,000 for the remainder interest. At the parent’s death, the child would own the $200,000 home.
- Purchase a life estate in the child’s home. The flip side of the sale of a remainder interest is for the parent to purchase a life estate in the home of the child. Again, the federal government’s life estate tables are used. If the child has a home with equity of $200,000 and the parent is age 75, the parent can pay the child $104,000 in exchange for a deed granting him or her a life estate in the home. The parent must actually move into the home and reside there for at least one year. If there is a mortgage on the home, this would reduce the equity purchased by the parent. Consideration also must be given to the “due on sale” clause in the child’s mortgage and to capital gains tax liability.
- Reverse mortgages. In many instances, children provide financial support to their parents to bridge the gap between the parent(’s/s’) income and the parent(‘s/s’) expenses. In order to ensure that these funds will be repaid if the parent ever requires long-term care, it is good practice to record a mortgage against the parent’s estate to secure the funds advanced by the children.
Medicaid estate recovery
At the death of a Medicaid recipient, the state is entitled to recover from his or her estate. In New Jersey, an estate includes all assets in the name of the decedent, as well as assets in which the decedent had an interest through joint tenancy, tenancy in common, right of survivorship, a living trust, or another arrangement. Effectively, this means that if a husband and wife own a home together and the husband is a Medicaid recipient, at his death, Medicaid can file a lien on the home. If the home is owned as tenants by the entirety, which is the usual way married couples own homes, the lien will be for 100% of the value of the home. In Pennsylvania, estate recovery is limited to the probate estate. The recovery will be for all Medicaid benefits received after age 55. No recovery will be made if there is a surviving spouse or a surviving child who is under age 21, blind, or permanently and totally disabled. Life estates established during the parent(’s/s’) lifetime are exempt from estate recovery. Recovery cannot be made against the estate of the surviving spouse. If a lien is placed against the home, the spouse will not be forced from the home, but Medicaid will want payment if the home is sold or the spouse dies.
WHAT TOOLS ARE AVAILABLE FOR LONG-TERM CARE PLANNING?
- Asset protection plan. An asset protection plan is designed to help you achieve your goals despite the barriers erected by Medicaid and tax laws.
- If you are married, you and your spouse probably have reciprocal wills, through which you leave everything to each other. When one spouse requires nursing home care, it is important to review existing wills. Generally, it is best to leave unchanged the will of the disabled spouse. However, the will of the other spouse should be revised so that, if he or she dies first, assets are not left to the disabled spouse.
- Living will. Your living will should be reviewed to ensure that it contains appropriate instructions regarding end-of-life decisions. Specifically, it should state the types of treatment you do or do not want in the event that you are either brain dead or terminal, and two physicians and a family member have agreed that there is no hope of your recovery.
- Power of attorney. Your powers of attorney should be reviewed for adequacy. Often, powers of attorney are missing such elements as the right to make gifts or do banking in accordance with the New Jersey Durable Power of Attorney Act. Additionally, many powers of attorney fail to include a reference to real estate that is to be sold. Prior to the sale of real estate, many title companies require that the street address and block and lot of the property be included in the power of attorney.
- Children’s trust. Establishing a trust for the benefit of children often offers tax advantages. It also can help to avoid the risk of making outright transfers to children, such as the risk of creditor actions or the loss of assets in a divorce.
- For most clients, the primary goal of long-term care planning is to protect their home. While many clients feel they should deed their home outright to their children, this often is not a good solution because of the risk factors and adverse tax effects. There are; however, a number of other strategies available to achieve this goal.
- Care agreement. If a child cares for a parent, it is possible for the parent to pay for that care, effectively transferring assets in a manner that will not trigger a Medicaid penalty. This must be done pursuant to a written care agreement.
WHAT SHOULD YOU KNOW ABOUT APPLYING FOR MEDICAID?
Medicaid applications are filed with the Board of Social Services for the county in which the care is being provided even if the applicant lived in a different county. Applicants must report all assets under penalty of perjury. The Board of Social Services has 30 days to approve or deny an application, but typically, the process takes about 60 days. Applicants have a right to appeal in the event of a denial. Medicaid can be granted retroactively for three months prior to the date of application if the Medicaid applicant was eligible at that time. Otherwise, eligibility begins on the first day of the month following the Medicaid application.
Medicaid eligibility rules are complex, and it is possible for errors to result in a delay in eligibility. In such cases, the facility must be paid by the family on a private-pay basis until Medicaid eligibility is granted. Given the potential for this outcome, many applicants choose to have an elder law attorney represent then during the application process. An elder law attorney also can help with periodic redeterminations for Medicaid eligibility. These occur annually for recipients on the Medicaid Only program and every six months for those on the Medically Needy program.
WORKING WITH BEGLEY LAW GROUP
For over 70 years, the attorneys of the elder and disability law firm Begley Law Group have been dedicated to helping clients plan for long-term care concerns. We have expertise in all aspects of elder law and provide clients with the most up-to-date information and advice. The firm participates in the formulation of legislation related to elder law issues. We also advocate for the rights of seniors on both national and state levels.
Clients requiring long-term care planning can benefit from our Asset Protection Planning program, designed to help identify goals and find the best strategies and solutions for achieving them. At the initial meeting, we will discuss your situation and ascertain your needs. We will then advise you of our fee, which is a flat rate that covers everything within the scope of the service.
LONG TERM CARE SELF-DIAGNOSTIC TEST
Many clients involved in long-term care planning find it useful to complete the following Self-Diagnostic Test. Please take a few minutes to answer these questions.
1. Am I willing to risk all that I have accumulated through a lifetime of hard work and disciplined saving, including my home, my car, and all of my liquid assets, rather than take the time to plan for the future? □ Yes □ No
2. Do I understand that the cost of planning is insignificant when compared to the cost of paying for long-term care? □ Yes □ No
3. Do I understand that the risk of my needing some form of long-term care (e.g., home care, assisted living, nursing home care) is roughly 70%? □ Yes □ No
4. Do I know what long-term care will cost? $________________
5. Do I know how I will pay for that care if I need it?____________________________________________
6. Do I know what the impact will be on my spouse and children if I spend $100,000 ± per year on long-term care?__________________________________________________________________________
7. Should I explore the possibility of buying long-term care insurance? □ Yes □ No
If no, why not?___________________________________________________________________________
8. Should I hope this problem never arises and ignore it? □ Yes □ No
9. Should I take steps to try to protect my life savings now? □ Yes □ No
What are my reasons for these decisions?____________________________________________________
________________________________________________________________________________________
10. Do I understand that if I become sick, it may be impossible for my spouse or children to care for me, regardless of how much they are committed to doing so? □ Yes □ No
11. Are my wills, trusts, living wills, powers of attorney and other legal documents up to date? □ Yes □ No
The post Planning for Long-Term Care first appeared on SEONewsWire.net.]]>
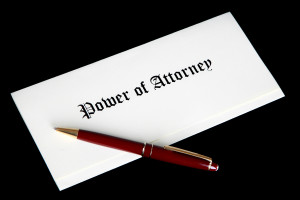
Durable Powers of Attorney
There is a need in all of us to nurture our parents as they become older. We make decisions regarding where they will live – whether in their own home, with you or in an elder care facility. After making this decision, however, you find there are other preparations to arrange. You may now find yourself in charge of such financial and medical matters as overseeing their insurance and day-to-day concerns like paying the bills. This is where durable powers of attorney can change things and pave the way for both you and your parent to have smoother transitions on all necessary legal matters.
Durable Power of Attorney in Michigan
A durable power of attorney enables your elderly parent (called the “principal” in the power of attorney document) to appoint an “agent,” (you), to handle specific health, legal and financial responsibilities. This document is especially important in regards to their healthcare. With the need for proper medical assistance becoming such an important issue, being able to step in and make decisions regarding your parent’s care, and their benefits under the Affordable Care Act, is vital. For instance, under this act, seniors with Medicare benefits will never have them reduced or eliminated and, will always be able to choose his or her own doctor. This is why it is essential to know what their rights are and set up the legal means to take over, if necessary, and make decisions for them before they become forgetful, terminally ill or have difficulty handling these tasks. By doing this now, while your parent is capable of deciding to seek assistance:
- First: the transfer of responsibilities occurs immediately.
- Second: if they do unfortunately, become incapacitated or incompetent, this will allow you to make many important financial decisions, pay bills and make important healthcare decisions on their behalf.
- Third: this provides an opportunity to do crucial Medicaid planning. What this means is that if your parent should need long-term care in the future, which is expensive, this can deplete their life savings before they are even allowed to become eligible for benefits such as Medicaid or Medical Assistance. Through this planning, you can help your parent protect the assets they have; including their home.
Not All Durable Powers of Attorney are Equal
One of the big issues Michigan families run into is that not all durable powers of attorney are created equal. Quite often when a durable power of attorney is reviewed it is prepared from an estate planning perspective, not an elder law one. Meaning there are limitations that won’t allow you to properly plan for VA Benefits or Medicaid because the power of attorney was drafted by someone who is not a Certified Elder Law Attorney.
Durable Power of Attorney for Your Parents
We understand that emotions involved while caring for your elderly parent can seem almost as overwhelming as the financial obligations themselves. As your loved ones age, together, we can plan a caregiving strategy. By choosing The Elder Care Firm, a practice that is dedicated to helping Michigan seniors, veterans and their families plan for and cope with the many issues that come with growing older, this will help smooth transitions and give you a better view of the scope of your responsibilities. To learn more about the durable power of attorney and speak with a lawyer who can help, please contact us today for more information.
The post Durable Powers of Attorney Can Help Smooth Transitions for Elder Care in 2015 appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Durable Powers of Attorney Can Help Smooth Transitions for Elder Care in 2015 first appeared on SEONewsWire.net.]]>Medicare supplement leads, whether they are exclusive or not, require some fact checking first. For example, a fair number of lead generation companies suggest they are offering real-time leads, but in reality, they are only selling information garnered from a generic health insurance form. Anyone over 65 that fills out an online form is fair game and considered to be a lead. And while they technically are leads, they may not be leads looking for Medicare supplement quotes.
Many online lead generation companies claim they offer real-time Medicare supplement leads, and some even go as far as to claim they are exclusive leads. How does one sort through all the claims and make a determination about their veracity? And how are the leads generated?
To effectively build a thriving insurance company, working with a lead generation company can help to navigate these questions. Such a company provides leads using a dedicated Medicare supplement insurance form, which specifically asks if the individual is looking for Medicare supplements, if they are looking for Medicare Advantage or Medigap, and if they are already covered by Medicare Parts A & B. Those receiving these leads know right away that these potential customers are quite serious about buying Medicare supplements and calling them is easy with the information provided.
Another important point to consider is how the lead generation company gathers their leads. Interested parties should check to see if the company garners their Medigap, Medicare or Medicare Advantage leads the same way they generate health insurance leads. If they do blanket marketing (search and email marketing) for people wanting “health” insurance, this is an ineffective strategy that will likely generate dud leads. Health insurance is not the same thing as Medicare supplement insurance.
The most desirable tools in an agent’s arsenal are Medicare supplement leads from a lead generation company that uses a dedicated Medicare form. Anything else is a waste of time and money.
Benepath is the leading provider of exclusive medicare leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Making Sure Medicare Supplement Leads Are Genuine Before Purchasing first appeared on SEONewsWire.net.]]>Now, a Rand Corporation study has examined the data and found that the theory is unsupported by the evidence. Placing limits on medical malpractice lawsuits does not reduce the volume or cost of emergency room care.
The study, published in the New England Journal of Medicine, analyzed data from emergency rooms in South Carolina, Georgia and Texas, three states that put strict limits on medical malpractice claims in the past decade.
All three states raised the bar for a medical malpractice claim for emergency care to “gross negligence,” meaning, basically, that doctors had to actually know that they were providing improper care, but provided it anyway. Researchers compared metrics on defensive medicine procedures and costs for Medicare claims in these states, compared to states that did not have higher bars for malpractice claims. Overall, the study found no reduction in the metrics studied. There was only a small reduction in one metric, charges per patient, in one state.
Bob Briskman is a Chicago malpractice attorney with Briskman Briskman & Greenberg. To learn more call 1.877.595.4878 or visit http://www.briskmanandbriskman.com/.
The post Study finds that stricter limits on medical malpractice lawsuits do not reduce healthcare costs first appeared on SEONewsWire.net.]]>Medicare Advantage enrollees have through February 14, 2015 to withdraw from their Medicare Advantage plan and instead receive Medicare Parts A and B through Original Medicare. During this period, recipients can also join a Prescription Drug Plan (PDP) if necessary. There are some issues that individuals should keep in mind if they would like to withdraw:
- During the Medicare Advantage Disenrollment Period (MADP), it is not possible to switch to another Medicare Advantage plan – the only option is to go to Original Medicare coverage Part A and Part B. Those who would like to switch Medicare Advantage plans may do so during Fall Open Enrollment, which runs from October through December.
- Individuals returning to Original Medicare should consider how they might manage the deductibles, coinsurance and copayments they may encounter when seeking medical care and coverage. For example, individuals seeking to purchase a Medigap policy may face higher premiums or a waiting period.
- Keep in mind, if you drop other coverage (i.e. employer or union health care coverage), you may not be able to reinstate your coverage.
To learn more about these Medicare click here: http://www.medicare.gov/
Learn more about our services at Littman Krooks by clicking here.
Was this article of interest to you? If so, please LIKE our Facebook Page by clicking here.
The post If You Want to Withdraw from Medicare Advantage first appeared on SEONewsWire.net.]]>An example of insurance products that hold little appeal to people is final life expenses. This is a demographic that needs to be approached when the timing is right for the customer.
Typically you’d target this niche by age and health factors. An example would be a 67-year-old male with diabetes about to go to hospital for a possible amputation. This individual may be very interested in final expense insurance. In other words, if you’re buying targeted leads, target older individuals with health issues. You can filter for those kinds of leads by asking your lead generation company.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Don’t know what to write about when it comes to insurance article marketing? first appeared on SEONewsWire.net.]]>Today, a career in the insurance industry is a wise choice, particularly if you sell Medicare supplements. They are the main staple of many thriving insurance agencies. Those agencies that have built their customer base using Medicare supplement leads know that no matter how many leads they get, they always need more. Agents always want to have other lead generation techniques in their marketing arsenals.
Cold calling may be dead as a trend, but it actually does work for some agents. Those with a knack for engaging people in conversations find it easy to discuss just about anything with their potential customers, including what type of insurance they need to protect their health. Ease with the topic paves the way to a greater rapport between an agent and a lead, and a knowledge of the product allows agents to sell what they know would work for prospects with confidence.
In addition to sourcing pre-screened leads from a reputable lead generation company, other tried, tested and true tactics may include use of free classified ads, message boards, an agent’s website, Twitter, Facebook, Tumblr and other social media platforms. Agents should make sure to tailor the message to each medium and to write succinctly. It can be a big task, but making a pitch or posting information on Twitter comes easily for those who know their products. If written eloquence poses a challenge, agents can hire the work out.
However, an interested agent should note that some of the Medicare supplement leads found via social media and other methods may not be of the highest quality. Expand beyond one lead generation method. Combine social media and purchased leads for a solid, blended marketing strategy that provides leads on a daily basis.
Those who have an agency or personal agent’s website should make certain it is up-to-date with the latest information and looks fresh, appealing and clean. The site should be easy to load and should contain relevant information for seniors searching for Medicare supplement insurance. With a clean and functional website, a business can grow exponentially. A website gives an agent the opportunity to explain insurance jargon in plain English and to tell people what they need to know to make informed decisions about which Medicare supplements are the best fit.
Agents should treat each potential customer as if he or she were already a customer. A successful agent will go the extra mile to help someone choose the right supplement. The post Medicare Supplement Leads Come in Many Forms first appeared on SEONewsWire.net.]]>
If you have been in the insurance business for any length of time, you have likely learned there is an enormous difference between working hard and working smart – but that the two can go together.
Working hard often means nose to the proverbial grindstone while not always making progress. New agents are familiar with the struggle of working hard to find leads but failing to make headway. Those who work smart know the ins and outs of selling insurance, make smart marketing decisions and buy life insurance leads from a lead generation company. Fortunately, even a new agent can buy life insurance leads that are pre-screened, connecting the agent with clients who are virtually ready to invest money in a policy.
No one said selling life insurance was going to be easy. People are not fond of the idea of insurance, and many go out of their way to avoid it even after agreeing that they need it.
Those agents who have chosen to work life insurance, final expense insurance or group insurance tend to find that the prevailing economy greatly affects whether people are interested in buying a policy. In times of economic instability, selling anything other than Medicare supplement insurance can be an uphill battle. As such, it is a smart marketing decision is to offer more than one kind of insurance policy and broaden your business base.
When one potential market goes dry or stagnant, having a back-up, captive market choice like Medicare and Medicare supplements is one of the only ways to remain stable with a decent income.
Sourcing good leads may create some anxiety, but it does not have to. Lead generation companies can provide fresh, real-time leads daily – if they are your choice. Make sure to choose a reputable company like Benepath. Benepath has been in the insurance business for many years, and the company knows what it is doing.
It is hard work keeping track of various leads in the niches you want to grow, but it’s smart marketing at the same time.
Benepath is the leading provider of exclusive life insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Work Hard or Work Smart? Life Insurance Leads Can Be Found Anywhere. first appeared on SEONewsWire.net.]]>If you want to educate your readers about Medicare and Medicare supplements, just spell it out in small, easy to understand chunks. The technical details are not what people are looking for. Their main interest in Medicare is how it benefits them. The technical end of things is up to you to handle behind the scenes.
Most people want the bottom line first, which is usually how something benefits them. Next, they want to know how much it is going to cost. Open enrollment and other insurance issues, such as the donut conundrum, are at first not comprehensible to most. Break it down, walk them through it and keep it simple. If you can capture people’s attention with well thought out, easy to read articles, you are one step ahead of the competition.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post When article marketing, try not to sound like you are selling something first appeared on SEONewsWire.net.]]>But aggressive selling has no place in online insurance sales. T
here are a number of reasons for that, but we’ll only outline two.
Your target demographics do not tolerate aggression in sales people. Let’s say you sell Medicare policies and Medicare supplements to an older demographic. For an older person, it can be frightening when a salesperson tries to ram a policy sale through before the individual knows what is happening. Many seniors take time to think through things — not always because of cognitive issues, but because of personal preferences. As such, you must tailor your sales pitches to the people to whom you sell.
Additionally, do not view what you have to say to your prospective clients as a “pitch.” You need to strive for genuine interest. Really get into a one-on-one conversation with people. Avoid speaking down to prospective clients, honor their questions, answer them honestly, give them the information they need and always keep your word when you say you will do or send them something.
This routine also applies to younger crowds considering life insurance. Aggression is a huge turn-off. Just don’t do it.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Sell with passion, not aggression first appeared on SEONewsWire.net.]]> When a Medicare beneficiary is hospitalized, whether you are coded as “admitted” or under “observation” makes all the difference in the world if you are looking at Medicare paying any cost of care for your rehab in a nursing home in Michigan.
When a Medicare beneficiary is hospitalized, whether you are coded as “admitted” or under “observation” makes all the difference in the world if you are looking at Medicare paying any cost of care for your rehab in a nursing home in Michigan.
I just finished my Wester Michigan University-Cooley Law School student finals and as part of the final exam I had a question regarding a loved one being in the hospital for observation for 3 days then needing 2 months of rehab. The crux of the issue was how Medicare treats people who are in a hospital for observation versus being admitted to the hospital.
The difference is whether Medicare will pay any cost of care for the rehabilitation.
Access, Area Agency on Aging 1-B newspaper had a great article discussing this as well.
Medicare Part A Coverage of Rehab
If you are on Medicare Part A and spend 3 midnights in a hospital and are admitted you can have part of your rehabilitation in a nursing home covered by Medicare. Medicare will pay 0-20 days with zero out of pocket coast. 21-100 days you may have a co-pay of $152 per day or supplemental insurance that will pick up the slack. After 100 days Medicare runs out, and to re-qualify for rehab, you need to go 60 days without a claim.
Medicare Requires “Admittance” to Cover Rehab
It can be confusing the difference between observation and admittance, but it’s important to understand the difference. Medicare Part A will only cover the rehabilitation following a hospitalization if a patient is classified as admitted for at least three consecutive midnights at the hospital. The time spent under observation does not count towards the requirement.
Hospitals Push More To “Observation”
According to the Center for Medicare and Medicaid Services, there’s been more than 300% increase in hospital observation care stays from 2006 to 2010.
What this means is that families will need to really push the hospital to getting admitted versus just being under observation.
The post Medicare Tip: How being “Admitted” versus under “Observation” at the Hospital Makes All The Difference appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Medicare Tip: How being “Admitted” versus under “Observation” at the Hospital Makes All The Difference first appeared on SEONewsWire.net.]]>Medicare only pays for care in a nursing facility if a patient is admitted to the facility within a month of having been admitted to a hospital for at least 3 consecutive days. In addition, Medicare requires physician certification of the fact that the necessary care can only be provided by an inpatient facility. The Centers for Medicare and Medicaid Services (CMS) must have approved the facility.
For Medicare to cover care in a skilled nursing facility, the patient must need the facility’s rehabilitation services five days a week, or its skilled nursing services seven days a week. If the care could be administered at home by a nurse on a less frequent basis, Medicare will not cover the care in a facility.
Even when care in a facility is covered, Medicare only pays for 100 days of care. For the first 20 days, full coverage is provided. From days 21 through 100, co-payment is required. After 100 days, the patient is required to pay privately until they have exhausted their resources and are eligible for Medicaid.
Medicare charges are monitored by Recovery Audit Contractors, who work for the CMS. These contractors receive a commission for detecting and recovering overpayments, so doctors and hospitals are very motivated to avoid charging Medicare for expenses that are not covered.
The elder law attorneys at Hook Law Center assist Virginia families with will preparation, trust & estate administration, guardianships and conservatorships, long-term care planning, special needs planning, veterans benefits, and more. To learn more, visit http://www.hooklawcenter.com/ or call 757-399-7506.
The post What is covered by Medicare in a skilled nursing facility? first appeared on SEONewsWire.net.]]>As a professional servicing seniors for the past 10 years, I have recognized the importance of clarity of information for both caregivers and seniors to properly discern the services that are needed both immediately and in the future. My analogy has always been that, when you are young parents, you have no clue as the choices, cost and requirement of child care services until you are there frantically calling around searching for the right options that are both safe, convenient and within your budget.
The same holds true for senior care. People rarely plan in advance for the choices that seems so far off into the future. Let me begin by explaining Home Care options.
Although most forms of home care are bundled into that one phrase, there are extreme differences when comparing, medical and non-medical options.
Non-medical home care is basically caregiving paid on an hourly basis to provide general assistance with activities of daily living. These might include assistance with cooking, cleaning, showering or even medication assistance. This type of home care is paid for privately with typically a minimum number of hours per day or week required by the provider.
Medical home care, also referred to as skilled nursing care, includes providing nursing assistance along with physical/occupational and speech therapy if needed. Home Health Care is paid for by either Medicare/Medicaid or a private insurance if the eligibly is met. The criteria includes:
• Doctor’s orders for referral
• The patient is having difficulty leaving the home without assistance (home bound)
• A change in medical status
If the patient meets this criteria, then a nurse will go to the patient’s home to evaluate, treat and educate them to eliminate a relapse or readmission into the hospital.
To better explain medical home health care, here is a complete explanation provided by Medicare.gov establishing what it is and what to expect:
What is home health care?
Home health care is a wide range of health care services that can be given in your home for an illness or injury. Home health care is usually less expensive, more convenient, and just as effective as care you get in a hospital or skilled nursing facility (SNF).
Examples of skilled home health services include:
• Wound care for pressure sores or a surgical wound
• Patient and caregiver education
• Intravenous or nutrition therapy
• Injections
• Monitoring serious illness and unstable health status
The goal of home health care is to treat an illness or injury, to regain your independence, and become as self-sufficient as possible.
If you get your Medicare benefits through a Medicare health plan, check with your plan to find out how it gives your Medicare-covered home health benefits.
If you have a Medicare Supplement Insurance (Medigap) policy or other health insurance coverage, tell your doctor or other health care provider so your bills get paid correctly.
If your doctor or referring health care provider decides you need home health care, they should give you a list of agencies that serve your area, but must tell you whether their organization has a financial interest in any agency listed. The decision on what agency to select is the patient or family choice.
What should you expect from home health care?
• Doctor’s orders are needed to start care. Then the home health agency will schedule an appointment and come to your home to talk to you about your needs
• The home health agency staff will also talk to your doctor about your care and keep your doctor updated about your progress.
Examples of what the home health staff should do include:
• Check what you’re eating and drinking.
• Check your blood pressure, temperature, heart rate, and breathing.
• Check that you’re taking your prescription and other drugs and any treatments correctly.
• Ask if you’re having pain.
• Check your safety in the home and teach you how to take care of yourself
• Coordinate your care with Physician
The post Home Health Services…What Does it Include? appeared first on Estate Planning Lawyers | Elder Law Attorneys | Brighton | Novi | Livonia Elder Law Attorneys.
The post Home Health Services…What Does it Include? first appeared on SEONewsWire.net.]]>Study your demographics. If you are marketing to retired seniors or to middle-aged executives, narrow down where they live. If you market Medicare to seniors,for example, locate areas with higher concentrations of retirement homes, private care homes or assisted living facilities. Aim any snail mail campaigns in that direction.
Middle-aged executives who fall within a certain age range are more likely to consider life insurance, term insurance or final expense insurance. Select the age range you want to market to and design your ad campaign accordingly. It still takes some guesswork, but persistence will convert customers.
You may be marketing to collateral niches, but it does not really matter. If someone is interested in your marketing material, you will get a call or email. Intelligent techniques will reward you.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Only market to interested people first appeared on SEONewsWire.net.]]>CMS has released the Medicare and Medicaid numbers for 2015. They are as follows:
Medicaid
- Income Cap[1] $2,199
- Maximum Community Spouse Resource Allowance (CSRA)[2] $119,220
- Minimum CSRA[3] $23,844
- Maximum Minimum Monthly Maintenance Needs Allowance (MMMNA)[4] $2,980.50
- MMMNA (July 1, 2014 until June 30, 2015)[5] $1,966.25
- Excess Shelter Allowance (July 1, 2014 until June 30, 2015)[6] $589.88
- Maximum Resource Limit (Individual)[7] $2,000
- Minimum and Maximum Cap on Equity in the Home[8] $552,000 – $828,000
Medicare
Part A
- Medicare Co-Payment – Skilled Nursing Facility (SNF)[9] $157.50
- Hospital Deductible[10] $1,260
- Per day Co-Insurance – Day 61 -90[11] $315
- Per day Co Insurance – Day 91-150[12] $630
Part A Premium (for voluntary enrollees only)
- With 30-39 quarters of Social Security coverage[13] $234
- With 29 or fewer quarters of Social Security coverage[14] $407
Part B
Medicare Part B – Single or Married and Filing Separate Return
Part B Income-Related Premium[17]
| Beneficiaries who file an individual tax return with income: | Beneficiaries who file a joint tax return with income: | Income-related monthly adjustment amount | Total monthly premium amount |
| Less than or equal to $85,000 | Less than or equalto $170,000 | $0.00 | $104.90 |
| Greater than $85,000 and less than or equal to $107,000 | Greater than $170,000 and less than or equal to $214,000 | $42.00 | $146.90 |
| Greater than $107,000 and less than or equal to $160,000 | Greater than $214,000 and less than or equal to $320,000 | $104.90 | $209.80 |
| Greater than $160,000 and less than or equal to $214,000 | Greater than $320,000 and less than or equal to $428,000 | $167.80 | $272.70 |
| Greater than $214,000 | Greater than $428,000 | $230.80 | $335.70 |
In addition, the monthly premium rates to be paid by beneficiaries who are married, but file a separate return from their spouse and lived with their spouse at some time during the taxable year are:
| Beneficiaries who are married but file a separate tax return from their spouse: | Income-related monthly adjustment amount | Total monthly premium amount |
| Less than or equal to $85,000 | $0.00 | $104.90 |
| Greater than $85,000 and less than or equal to $129,000 | $167.80 | $272.70 |
| Greater than $129,000 | $230.80 | $335.70 |
Standard Part D Cost-Sharing for 2013[18]
- Annual Deductible Maximum $320
- Member Pays 25% of the Next $2,640 25% = $660
- Initial Benefit Period Maximum $2,960 ($320 + $2,640)
- Donut Hole Threshold $3,720
- Catastrophic Coverage $4,700 ($320 + $660 + $3,720)
- Catastrophic cost-sharing: Generic $2.65 or 5% (whichever is greater)
- Catastrophic cost-sharing: Brand $6.60 or 5% (whichever is greater)
[1] 42 U.S.C. §1396a(a)(10)(A)(v); 2015 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[2] 2015 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[3] 2015 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[4] 2015 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[5] 79 Fed. Reg. 3593 (Jan. 22, 2014).
[6] 79 Fed. Reg. 3593 (Jan. 22, 2014).
[7] 20 CFR § 416.1205(c).
[8] 42 U.S.C. §1396p(f); 2015 SSI and Spousal Impoverishment Standards, www.medicaid.gov.
[9]Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[10] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[11] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[12] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[13] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[14] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[15] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[16] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[17] Medicare 2014 & 2015 Costs at a Glance, www.medicare.gov.
[18] http://www.medicareadvocacy.org.
The post MEDICAID AND MEDICARE 2015 COLA NUMBERS first appeared on SEONewsWire.net.]]>If you’re selling Medicare supplements and/or Medicare, you are aiming at a certain audience. Most are tech savvy, though some are not (and some are in between and faking it). This is where you come in. Your audience informs the best way to market your products. Email campaigns, texting and tweeting about your products may work well with about 25 percent of your intended prospects. What about the other 75 percent?
If you know how your customers want to receive information, you have their attention. Some seniors prefer getting information in the mail. It is familiar. Posted mail gives people the time to sit, read and digest the information in their own good time before making a decision. Not all older Americans have a computer in the house. Some who do only use it for emails to grandchildren.
Tech-smart seniors do appreciate communication via the latest gadgets they own. Provide this part of your audience with the information they requested quickly and professionally.
Contemporary marketing allows you to use multiple methods to suit different parts of your audiences.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Trying to find leads on your own? first appeared on SEONewsWire.net.]]>Experts in patient safety say that misdiagnosis, which can include delayed, missed or incorrect diagnoses, may affect between 10 and 20 percent of all cases.
Medical errors that harm patients and are the result of negligence on the part of doctors or hospital personnel may give rise to medical malpractice lawsuits. However, in the vast majority of misdiagnosis cases, lawsuits are not filed. In many cases, patients are not aware that an error was made because the misdiagnosis is never reported.
A report by Daniel R. Levinson, the inspector general of the Department of Health and Human Services, found that only one in seven mistakes or injuries involving Medicare patients are actually reported by hospital staff, even though reporting events that cause patients harm is a requirement of receiving Medicare payments.
Patients who suspect a misdiagnosis caused or worsened an injury should consult with a medical malpractice attorney to determine whether a lawsuit is appropriate to recover compensation for the harm they suffered.
Paul Greenberg is a medical malpractice lawyer in Chicago and malpractice attorney with Briskman Briskman & Greenberg. To learn more call 1.877.595.4878 or visit http://www.briskmanandbriskman.com/.
The post Many misdiagnosis errors go unreported first appeared on SEONewsWire.net.]]>Think TV commercials. If you’ve ever watched a great show on Hulu and had it interrupted every ten minutes with the same commercial, over and over, you know the true definition of irritation.
If you over-promote a product, your presence can become annoying and delete-worthy. Instead, make it a point to send your promotions to the right crowd in a timely manner. Avoid promoting Medicare supplement insurance to the 20-something crowd, for instance.
Pay attention to what and where you are marketing, and give your customers plenty of time between postings to respond to you.
Benepath is the leading provider of exclusive group health insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Social media is a good communications vehicle, but don’t overuse it on your group insurance leads first appeared on SEONewsWire.net.]]>But reform is stalled for more reasons than politicians mention or protests denounce. Some we can guess, based on each party’s philosophy. Other reasons, however, have more to do with cost analysis than compassion.
A recent report authored by Robert Rector and Jason Richwine of the Heritage Foundation took an in-depth look at the economic ramifications of immigration reform. Their key argument points to a damaging effect on U.S. taxpayers.
Government benefits are distributed lopsidedly, they say. Rector and Richwine suggest that each year, undocumented immigrants collect government benefits to the tune of $54.5 billion.
The report claims that the average American household receives $31,584 yearly in benefits between local, state and federal resources.
Heads of households who have a college education receive, on average, $24,839 in benefits, and they pay $54,089 in taxes. The government nets $29,250.
Heads of households who have less than a high school education, however, receive $46,582 in benefits, and they pay only $11,469 in taxes. The net “deficit” to the government is $35,113. All American taxpayers are footing that deficit. Not many are even aware of how large the gap is.
The large economic gap that education levels create is important to the immigration debate, as nearly 50 percent of illegal immigrants have less than a high school education. Only about 25 percent have completed study equivalent to high school or hold a diploma. Though they may contribute to the economy in other ways, many under-educated, undocumented workers simultaneously drain it.
Philosophical and political differences aside, the nation is already united in supporting under-educated, illegal immigrants though heavy tax imbalances. And if the number of immigrants with less education who are allowed to enter the country increases (whether through immigration reform or another route), the economic gap will escalate.
If undocumented immigrants become legalized residents of the United States, they will eventually have access to all government benefits. Unfortunately, because of the average balance of benefits to tax in many of these households, national benefit costs for the (then) documented immigrants would rise to approximately $106 billion yearly. Upon retirement with access to Medicare and Social Security, benefits would hit $160 billion.
Compassion for this first generation of illegal aliens has the potential to generate $6.3 trillion in lifetime government costs in benefits.
Compassionate immigration reform, based on the Heritage Foundation report numbers, should not be free. Policymakers must find a way to reach out to those crossing its borders without harming its current citizens.
The post Compassionate Immigration Reform Should Not Come for Free first appeared on SEONewsWire.net.]]>
The term “aging in place” is being heard more frequently these days. Simply put, “aging in place” means remaining in your own home and maintaining your independence as you grow older. Some Americans hope to accomplish this entirely on their own; others assume they will have the aid of nearby family members. But there is another option. By joining a local aging-in-place organization older adults are now finding they can have the best of both worlds – the privacy and autonomy they value plus peace of mind from belonging to a community of people who are willing to step in to lend a hand when needed.
To date there are 145 such organizations (frequently referred to as “Villages”) already operating around the country. These nonprofit groups have proved so popular that 125 more are in development. There are ten “Village” in New York State, with seven more on the way.
One such group in Westchester County is At Home on the Sound. Serving Larchmont and Mamaroneck, At Home on the Sound is currently comprised of 150 members (ranging in age from 62 to 100), plus approximately 80 community volunteers of all ages. Many of At Home’s members are also volunteers. Besides providing enriching programs and activities, At Home on the Sound matches the volunteers with members who need local transportation or other assistance. In any given week At Home on the Sound provides 25 to 30 rides to doctor appointments, errands – even the nail salon!
At Home on the Sound volunteers are also available to handle simple household maintenance tasks like changing a hard to reach light bulb or fixing a leaky faucet. Several times throughout the year local high school students offer technology workshops providing one-on-one assistance to At Home members with cell phones and iPads. Staying up-to-date with technology not only has wonderful social benefits but can be a matter of safety as well. An occupational therapist offers free home safety assessments, while a volunteer Medicare expert conducts annual seminars to keep members up-to-date on laws and deadlines. Trained volunteer patient advocates are even available to accompany members to medical appointments.
At Home on the Sound schedules at least a dozen social and cultural programs each month for members. A gentle yoga class is offered every week. Lectures are held on a vast array of topics from Acupuncture to the Constitutional Convention. Bus trips are organized for outings to museums, Broadway shows, and concerts. Activities such as Scrabble, Bridge, foreign language conversation, and current events discussions bring together like-minded members for fun and intellectual stimulation. All the programs are designed to ward off the sense of isolation that can sometimes come with age.
Not only do aging-in-place organizations improve the lives of members, these nonprofits can also be a godsend for family members who live far away and may not have regular contact with their older loved ones. With a quick local phone call, the older adult who belongs to an aging-in-place group can easily access a ride or other assistance when needed.
Aging-in-Place organizations around the country offer similar services to enhance and improve the quality of life for older adults – and their families. To see if an aging-in-place organization is currently serving your area visit the Village to Village network for a searchable map of the US.
Learn more about At Home on the Sound by clicking here.
Was this article of interest to you? If so, please LIKE our Facebook Page by clicking here. Visit www.elderlawnewyork.com to learn more about helping seniors and their families plan for the future.
The post Aging Gracefully in Your Own Home – with a Little Help: Non-Profits Offer New Model for Growing Old on Your Own Terms first appeared on SEONewsWire.net.]]>For a number of years, direct mail was the go-to method to generate Medicare supplement leads. Cards were mailed out to specific target areas, and interested people replied asking for further information. From there, the agent made appointments and explained the various Medicare supplements available. The cards were and are nicely designed, attractive and well-written works of practical graphic design. They included postage paid for the return. If the cards captured a potential customer’s attention, and he or she asked you to call, half of your work was already done.
Some agents still find that direct mail really works well for them. Every insurance agent, especially newer ones, will not find them effective, but direct mail is still worth considering in combination with internet leads purchased from a lead generation company.
But you may also want to try buying leads from a lead generation company. When you call to order leads, you get an immediate list of pre-screened prospects who have expressed an interest in Medicare supplements. Communication can be instant. No more waiting for people to return cards that they may have lost or forgotten about. The leads you receive though the internet allow you to work in real time, make calls and set up appointments quickly. Exclusive leads are a bit more expensive than shared leads. However, the exclusive leads, which are only sent to you, convert at a higher ratio than working leads shared with several other agents.
Some agents still prefer direct mail because it works for them. However, if you have very little time to pursue this labor-intensive style of marketing, you may find buying leads from a lead generation company to be more lucrative, immediate and trustworthy. Certainly if you are in a hurry to make as many sales as you can, internet leads are a better time investment than mail cards.
Working online is simply the faster, easier way to build your insurance agency. The internet accelerates your ability to respond, make appointments and close sales.
Benepath is the leading provider of exclusive medicare leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post The Most Cost-Effective Marketing Route: Snail Mail Vs Internet Medicare Supplement Leads first appeared on SEONewsWire.net.]]>If your message doesn’t contain a call to action like, “Click here for further information on term life insurance,” potential customers have nothing to do. So of course they leave.
If you want to keep the relationship alive and fresh, get to your point right away. If you are doing a survey for a product, say so up front. If you are fishing for information to find an opening to talk about Medicare supplements, ask an indirect question. Ask the customer how they feel about recent changes in Medicare. If they do not understand it or know they lack coverage, you have found a concrete way to help them.
This isn’t hard work. It’s smart work.
Benepath is the leading provider of exclusive life insurance leads. To learn more, visit http://www.benepath.net or call 1-866-368-0377
The post Getting your message seen online: Part 6 first appeared on SEONewsWire.net.]]>
